Mold Related Illness Symptoms & Complaints
Mold Related Illness Symptoms & Complaints
- POST a QUESTION or COMMENT about possible symptoms of mold related illness & health complaints
My House is Making Me Sick?
This Mold Related Illness Guide provides a broad index of reports of health complaints or symptoms, of Illnesses that are either caused, or aggravated by indoor mold exposure or alternatively, that were believed or suspected by individuals to have a role in their physical or mental health complaints.
Here we provide descriptions and lists of ypes of mold reactions & list of Health complaints in moldy homes, lists of health complaints related to moisture or dampness and reports of those allergens & allergy illnesses in the home, types, causes, prevention. Health complaints by people sending mold samples to our laboratory. Photos of several Different-Appearing Mold-related Skin Rashes on People Not Suffering from Tinea
InspectAPedia tolerates no conflicts of interest. We have no relationship with advertisers, products, or services discussed at this website.
- Daniel Friedman, Publisher/Editor/Author - See WHO ARE WE?
Broad classes of reactions to allergenic, pathogenic, or toxic mold, allergens, and other indoor gases or particles
 Four Categories of Mold-Related Illnesses, Symptoms, or Complaints
Four Categories of Mold-Related Illnesses, Symptoms, or Complaints
In understanding how exposure to mold might cause or contribute to illnesses it is useful to distinguish among the meanings of the words allergenic, pathogenic, and toxic effects that exposure to something might explain.
Readers should not rely just on this document for medical diagnosis and instead should consult with their physician or with a specialist such as a medical toxicologist
- Allergenic - causing allergic Reactions - rhinitis, sinusitis, asthma, skin problems, other.
Quite a few of our clients reported non-Tinea (ringworm) skin rashes on exposure to high levels of mechanically disturbed molds, almost always during an amateur mold clean-up job, often apparently associated with Stachybotrys chartarum, and most immediately contacted on exposed (sometimes sweaty or moist) skin areas (neck, face, head, hands, arms) that were not protected during their mold cleanup project.
More examples of skin rashes that correlated in time of occurrence with significant indoor mold exposure are shown in this article
at DERMATITIS, SKIN RASHES,
and SKIN RASH FAQs. - Pathogenic - Produces Infections, caused by pathogens such as bacteria or viruses
- Mold Smell related Illnesses - headaches, vomiting, nausea, blocked noses, and asthmatic [MVOC's--DF]
- Toxic Illnesses - where mold is involved, may be produced by mycotoxins that are produced by some, not all, mold species. Note that even for a "toxic" mold species, the actual level of toxicity can vary significantlty depending on growing conditions such as the growth substrate (what the mold is feeding-on), humidity, moisture, and other factors.
- Respiratory Illnesses - asthma, COPD, etc.
- Digestive Tract Illnesses - liver diseases: fibrosis and necrosis; vomiting, diarrhea, intestinal bleeding
- Reproductive Illnesses - infertility, variations in reproductive and hormonal cycle
- Highly Serious Illnesses - Cancer, Tuberculosi, Lupus, Sudden Infant Death Syndrome (SIDS), Chronic Fatigue Disorder (CFS), Fibromyalgi, Epstein-Barr, aspergillosis
List of Mold Related Illnesses & Health Complaints
 This list of mold related illness symptoms and complaints is arranged alphabetically and begins just below.
This list of mold related illness symptoms and complaints is arranged alphabetically and begins just below.
This list is a combination specific, diagnosed medical illnesses and other anecdotally reported complaints associated with mold in buildings. Research to establish a firm chain of causation between mold and other indoor particles (or other substances) and these complaints in many cases has not been completed.
We capitalize names of known medical conditions. While the following list may be of assistance to some readers researching this topic, it should by no means be considered as scientifically authoritative nor complete.
Some complaints are listed here without any solid medical evidence regarding causation, if the complaints have been expressed to us by people investigating mold-related illness or building mold contamination. Such data should be considered for research purposes and not medically authoritative.
We are interested in adding to this list as well as providing succinct symptom lists associated with medically-diagnosed mold related illnesses. Suggestions and criticism are invited.
Also see MOLD RELATED ILLNESS GUIDE
Alphabetical Index to Symptoms of Mold Related Illnesses, Medical & Anecdotal
A - B - C - D - E - F - G - H - I - J - K - L - M - N - O - P - QR - S - T - U - V - WXYZ
Watch Out: this document is a mold-related symptom or complaint list, not a medical document.
This mold-illness-symptoms & complaints list does, however, collect both substantiated mold-related-illness complaints and a wide sampling of the nature and range of other complaints from people who believe or fear that mold or similar exposure has been a factor in their physical or mental health, a general reference for individuals or physicians interested in reading the nature and range of these complaints that may or may not actually be building or environment-related.
Can Mold Make You Sick?
We live in a sea of mold, and other stuff in the air we breathe, on cushions we sit on, clothes we wear, pools we swim-in, and so on. Most mold is not hurting anyone, and some of it makes us well when we're sick(Penicillium notatum, for example). Fear of mold (mycophobia) is unjustified and in our opinion, more a result of media hype, ENVIRO-SCARE, and gouging consumers.
A healthy person walking through a room of moldy air is not likely to die. On the other hand, there is a wealth of less rigorous empirical data matching occupant complaints with indoor mold and allergens.
Finally, for certain people, mold can be a serious problem if it's at high levels indoors. It's probably an overstatement by some authorities who assert that "... there are no proven links between mold and illness" - we refer readers to some of our lab's references for descriptions of illness-related molds, some of which are found in buildings.
See this separate
article MOLD RELATED ILLNESS GUIDE,
an Index to detailed articles aid in identifying illnesses that may be related to toxic or allergenic mold exposure. This is an atlas of mold related illness symptoms and complaints & of mold toxicity.
Readers needing a medical diagnosis of mold related illness should consult with their physician or with a specialist such as a medical toxicologist. If you need a specialist consult your family doctor and also
see MOLD DOCTORS - ENVIRONMENTAL MEDICINE
Alphabetic Index to Common Mold-related Illness Symptoms & Complaints
A
- Abdominal pain - also see Crohn's disease under C or inflammatory bowel disease under I
- Abnormal pap smears
- Acid reflux
- Acne
- Allergy symptoms (wide variety of), mild to severe and from transitory to chronic - Ref: Middleton and assoc.
- Allergic Bronchiopulmonary Aspergillosis (ABPA) - worsening of underlying asthma or cystic fibrosis,
coughing up blood, weight loss, fever, wheezing, muicous plugs produced by coughing - uncommon, occurs in persons with asthma and those with cystic fibrosis (CF) - Allergic Rhinitis and asthma are associated with responses mediated by immunoglobulin E (IgE)
- "Damp house linked to kids' risk of nasal allergies", New York Times, 1 Aug 2010
- Altered immunity
- Anaphylaxis
- Apnea, sleep
- Arsenic poisoning related to mold growth on antique wallpaper: Some antique green wallpaper pigments interact with some molds to release poisonous arsenic.
See details about arsenic related illness found
at ARSENIC HAZARDS at BUILDINGS & EXPOSURE HAZARDS for more about arsenic poisoning from this arsenic element in its gaseous form. A discussion of arsenic poisoning from Arsine Gas Exposure Hazards - Arsenic Hydride
More details are
at ARSENIC GREEN in WALLPAPER - green-pigmented wallpaper using arsenic green combined with mold growth releases toxic gases,discussed in our index to mold growths on building surfaces
found in our MOLD GROWTH on SURFACES, TABLE OF
Also see more abour arsenic poisoning found
at ARSENIC in WATER - Aspergilloma (fungal growth in lung), cough, cough, fever, weight loss. Uncommon. May be asymptomatic but show up in a lung X-ray in some patients who have a pre-existing lung cavity (e.g. due to T.B.), occurs in patients suffering HIV + pneumonia; coughing up blood is a serious and life thereatening condition;
- Aspergillosis, Chronic necrotizing Aspergillus pneumonia, or Chronic necrotizing pulmonary aspergillosis (CNPA) occurs in patients with an underlying disease such as COPD or alcoholism, symptoms include subacute pneu7monia, fever, cough, night sweats, weight loss.
- Aspergillosis, Invasive, occurs in patients who suffer from immunosuppression or prolonged neutropenia, leukemia, and others; symptoms include fever, cough, chest pain, difficulty breathing (dyspena), rapid breathing (tachypnea).
See ASPERGILLOSIS for details about the above Aspergillus-related illnesses.
- Asthma and asthmatic signs
- Asthma, adult onset
- Asthma, sudden onset, any age
- Asthma, increased symptoms or renewal of previously diminished symptoms
- Asthma due to fungal allergens: chest tightness, wheezing, cough, dyspnea. Worsens w/ exposure. Cx typically occur within 1 hr of exposure
2019/04/09 The New York Times reported a possible relationship between abnormally high levels of presence of the fungus Malassezia in the intestines and both the presence of and possibly improved treatment for inflammatory bowel disease including Chron's disease. - Rogers, Lakeigh, "You're Covered in Fungi. How's Your Health? Researchers explore potential contributors to inflammatory bowel diseases." The New York Times, 9 April 2019, p. D-6.
The article also cites possible connections between abnormally high levels of presence of the fungus Malassezia in the gut and asthma and also a possible association with prostate cancer.
B
- balance, loss of
- bladder and kidney pain
- Blastomycosis: "blasto" most-common in the U.S. in the Ohio and Mississippi river valleys, as far north as Minnesota. Can infect humans, causing both lung and skin infections infections ranging from asymptomatic to very serious
Saccente, Michael, and Gail L. Woods. "Clinical and laboratory update on blastomycosis." Clinical Microbiology Reviews 23, no. 2 (2010): 367-381.
Summary: Blastomycosis is endemic in regions of North America that border the Great Lakes and the St. Lawrence River, as well as in the Mississippi River and Ohio River basins.
Men are affected more often than women and children because men are more likely to participate in activities that put them at risk for exposure to Blastomyces dermatitidis. Human infection occurs when soil containing microfoci of mycelia is disturbed and airborne conidia are inhaled.
If natural defenses in the alveoli fail to contain the infection, lymphohematogenous dissemination ensues. Normal host responses generate a characteristic pyogranulomatous reaction.
The most common sites of clinical disease are the lung and skin; osseous, genitourinary, and central nervous system manifestations follow in decreasing order of frequency.
Blastomycosis is one of the great mimickers in medicine; verrucous cutaneous blastomycosis resembles malignancy, and mass-like lung opacities due to B. dermatitidis often are confused with cancer. Blastomycosis may be clinically indistinguishable from tuberculosis.
Diagnosis is based on culture and direct visualization of round, multinucleated yeast forms that produce daughter cells from a single broad-based bud. Although a long course of amphotericin B is usually curative, itraconazole is also highly effective and is the mainstay of therapy for most patients with blastomycosis. - bleeding lungs
- blood pressure irregularities
- body aches and muscle pains
- Boils and similar sores on skin, especially neck, but anywhere, of varying size and surface texture (smooth, scaly) especially following disturbance of moldy materials (S. chartarum)
(photos on file) - see Blastomycosis and Coccidioidmycosis
See also DERMATITIS - Breathing difficulties, - see Blastomycosis and Coccidioidmycosis
- Bronchopulmonary aspergillosis / allergic bronchopulmonary aspergillosis: inflammatory disease
caused by immunologic response Aspergillus sp.,
usually A. fumigatus, growing in bronchi of asthmatics
reported in immunocompromised patients and patients with chronic obstructive pulmonary disease (COPD)
and has been linked to building-related illness (BRI)
See ASPERGILLOSIS - bruising easily
- burning mouth
- burning eyes
- burning throat
- burning lungs
C
- Cancer - various, including prostate cancer
2019/04/09 The New York Times Rogers, Lakeigh, "You're Covered in Fungi. How's Your Health? Researchers explore potential contributors to inflammatory bowel diseases." The New York Times, 9 April 2019, p. D-6.
The article cites possible connections between abnormally high levels of presence of the fungus Malassezia in the gut and a possible association with prostate cancer. - Candida, systemic
Systemic candidiasis includes a spectrum of yeast infections caused by different species (types) of Candida.[1] It is a serious infection that can affect the blood, heart, brain, eyes, bones, or other parts of the body.
Although there are over 200 species of Candida, five different species of Candida cause 90% of systemic candidiasis.
The most common form of this invasive yeast infection is when Candida enters the bloodstream (candidemia). Signs of candidemia include fever and chills that do not improve with antibiotics. Symptoms of other types of systemic candidiasis depend on the organ or system which is infected.
Systemic candidiasis is the most common fungal infection among hosptilized people in high-income countries, including the United States. Diagnosis can be difficult, especially when the Candida is not found in the bloodstream.
Treatment usually includes consists of oral or intravenous (IV) antifungal medications
Common symptoms of candidemia (Candida infection of the bloodstream) include fever and chills that do not improve with antibiotics. Candidemia can cause septic shock and therefore may include symptoms such as low blood pressure, fast heart rate, and rapid breathing.
Systemic candidiasis may also affect other parts of the body such as the central nervous system (brain and spinal cord), abdomen, heart, kidneys, liver, bones, muscles, joints, spleen, and/or eyes.
Candidemia may be present, but not in all cases. Signs and symptoms depend on the organ or system infected.
For example, when Candida infects the eye, symptoms may include blurred vision with photophobia (the eye is overly senstive to light), whereas symptoms of candida endocarditis (Candida infection of the inner lining of the heart) may include fever, shortness of breath, fluid buildup in the arms or legs, tiny red spots on the skin, and weight loss.
Since many people who develop systemic candidiasis are already sick, it can be difficult to know which symptoms are from Candida infection and which symptoms are from complications of other medical conditions. - NIH, "Systemic candidiasis", retrieved 2017/10/16, original source: https://rarediseases.info.nih.gov/diseases/1076/systemic-candidiasis
Also see: Chronic Candidiasis FAQ - Dr. Fungus: doctorfungus.org/mycoses/human/candida/Chronic_Candidiasis.htm - Central nervous system disorders (CNS)
- Chest pain associated with excessive coughing
- Chills
- Choking
- Cholesterol or triglycerides unusual variations
- Chronic fatigue syndrome (CFS)
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), sometimes referred to as myalgic encephalomyelitis (ME) or chronic fatigue syndrome (CFS), is a debilitating disease that lacks a universally accepted case definition, cause, diagnosis, or treatment.
According to the CDC (link is external), more than one million Americans have CFS. At least one-quarter of individuals with ME/CFS are bedbound or housebound at some point in the illness and most never regain their pre-disease level of functioning.
ME/CFS strikes people of all ages and racial, ethnic, and socioeconomic groups, and is diagnosed two to four times more often in women.
The disease is characterized by at least six months of incapacitating fatigue experienced as profound exhaustion and extremely poor stamina, and problems with concentration and short-term memory.
It is sometimes preceded by flu-like symptoms followed by pain in the joints and muscles, unrefreshing sleep, tender lymph nodes, sore throat, and headache. A distinctive characteristic of the illness is post-exertion malaise, which is a worsening of symptoms following physical or mental exertion occurring within 12-48 hours of the exertion and requiring an extended recovery period.
Although the cause of ME/CFS remains unknown, symptoms may be triggered by an infection. - NIH, About ME/CFS, retrieved 2017/10/16, original source https://www.nih.gov/mecfs/about-mecfs
- Chronic sinus infections
- Chron's Disease, inflammatory bowel disease -
2019/04/09 The New York Times reported a possible relationship between abnormally high levels of presence of the fungus Malassezia in the intestines and both the presence of and possibly improved treatment for inflammatory bowel disease including Chron's disease. - Rogers, Lakeigh, "You're Covered in Fungi. How's Your Health? Researchers explore potential contributors to inflammatory bowel diseases." The New York Times, 9 April 2019, p. D-6. - Coated tongue
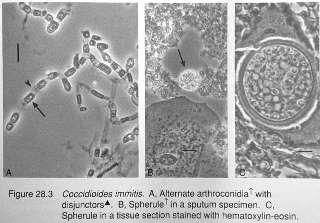
- Coccidioidomycosis - "cocci", most-common in Southwestern U.S. to California, West Texas to SOCAL, soil fungi infecting animals, can infect humans, causing both lung and skin infections ranging from asymptomatic to very serious
Symptoms: Valley Fever: cough, fever, fatigue, chest pain. History of travel to areas where the coccidioides soil fungus is found: southwestern United States, areas within Mexico and South America, also in south-central Washington.
Excerpt from U.S. CDC:
Valley fever, also called coccidioidomycosis, is an infection caused by the fungus Coccidioides. The fungus is known to live in the soil in the southwestern United States and parts of Mexico and Central and South America. The fungus was also recently found in south-central Washington.
People can get Valley fever by breathing in the microscopic fungal spores from the air, although most people who breathe in the spores don’t get sick. Usually, people who get sick with Valley fever will get better on their own within weeks to months, but some people will need antifungal medication.
Certain groups of people are at higher risk for becoming severely ill.
It’s difficult to prevent exposure to Coccidioides in areas where it’s common in the environment, but people who are at higher risk for severe Valley fever should try to avoid breathing in large amounts of dust if they’re in these areas. - retrieved 2016/08/18, original source: Valley Fever (Coccidiomycosis), U.S. CDC Centers for Disease Control & Prevention, Websitte: http://www.cdc.gov/fungal/diseases/coccidioidomycosis/ - Colds, recurrent
- Constipation
- Cough, dry hacking
- Coughing up blood
- Cryptococcosis:
Cryptococcosis is a fungal infection that typically affects people with HIV, cancer, or other conditions that weaken the body’s immune system.
The infection can progress to pneumonia and meningitis, which may cause serious symptoms of lung, brain, and spinal cord disease, such as headaches, fever, cough, shortness of breath, confusion, and weakness.
People who recover from cryptococcal meningitis often need long-term treatment with medication to prevent the infection from coming back. - NIH, retrieved 2017/10/16, original source: https://www.niaid.nih.gov/clinical-trials/cryptococcosis-study
D

- dandruff resistant to usual treatments
- dark urine
- death in extreme cases (humans, other animals)
- Depression
- Dermatitis: red, itchy skin, skin rashes.
The mold-related skin rashes shown at the top of this page, at left, and below in at SKIN RASHES and our SKIN RASH FAQs section illustrate patterns of skin rash suffered by some of our clients that appeared to be mold-related, usually following extensive mold-exposure or exposure of someone who was highly allergic to molds.
See also see Blastomycosis and Coccidioidmycosis - diarrhea
- difficulty concentrating
- difficulty in swallowing
- dirt-like taste in mouth
- Disorientation: several clients have reported disorientation, memory loss, language difficulties, and mood disorders that appeared to correlate with exposure to certain molds or MVOCs in their indoor environment.
- Dizziness
E
- endometriosis
- Eye infections, (beware of undiagnosed fungal eye infections), loss of vision
- eye irritation
F
- face flushing intermittent
- facial movements, unexplained twitching
- farmers' lung disease
- fevers
- fibrous discharge from the nose, nasal fibers, mucosa - (See Morgellon's syndrome or Morgellon's disease below)
- Fibromyalgia - numerous websites and articles discuss possible
connections between mold exposure and
Fibromyalgia - including these:
http://www.mold-survivor.com/fibromyalgia.html
http://www.swarthmore.edu/NatSci/SigmaXi/docs/PosterSummaries2003/zagory-
jessica.pdf#search=%22Fibromyalgia%20mold%20%22 - Swarthmore study
http://www.personalconsult.com/cgi-bin/htsearch - free clinical search
we have also corresponded with people who report suffering from Fibromyalgia and significant mold exposures, though the identification of genera/species and level of exposure were lacking. - Flu-like symptoms:
WARNING: flu-like symptoms can be a sign of potentially fatal carbon monoxide poisoning! Immediate help may be required. - Food allergies
- frequent bloody noses
- frequent infections
- Fungal infections, systemic such as Histoplasmosis, and Coccidioidomycosis, and Cryptococcosis, responding to contaminated bird droppings or construction dusts
G
- Glucan sensitivity: Glucans are glucose polymers that are components of most fungal cell walls, and exposure to airborne 13-beta-D-glucan has been known to cause irritation symptoms due to airway inflammation (7). However, these irritant effects are transient and self-limiting
H
- hair loss
- headaches
- heart attack
- hemorrhagic pneumonitis
- Extrinsic Allergic Alveolitis - (Hypersensitivity Pneumonitis) -
- heartburn
- Histoplasmosis - respiratory illness from airborne spores of Histoplasma capsulatum
Histoplasmosis is a disease caused when airborne spores of the fungus Histoplasma capsulatum are inhaled into the lungs, the primary infection site.
This microscopic fungus, which is found throughout the world in river valleys and soil where bird or bat droppings accumulate, is released into the air when soil is disturbed by plowing fields, sweeping chicken coops, or digging holes.
Histoplasmosis is often so mild that it produces no apparent symptoms. Any symptoms that might occur are often similar to those from a common cold.
In fact, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, since the body’s immune system normally overcomes the infection in a few days without treatment.
However, histoplasmosis, even mild cases, can later cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40. - Source: NIH, Facts About Histoplasmosis, retrieved 2017/10/16, original source https://nei.nih.gov/health/histoplasmosis/histoplasmosis
Question: is histoplasmosis grown or spread in sewage?
Can you tell me if it would be possible for histoplasma to grow in human waste? My daughter has been diagnosed with histoplasmosis and the rest of the family is awaiting test results. We have all had repeated severe respiratory symptoms including pneumonia and bronchitis.
My daughter has developed asthma and mine has worsened. Several months ago, our main sewer line backed up and flooded a heat vent in the floor. My house is on a concrete slab so cleaning the air duct was not an option, and my landlord has refused to help. I'm just curious if this fungus could have grown there, and we became infected by turning on the heat for the first time in September and releasing spores into the air.
I am a single mother who is now out of work due to my daughter's hospitalization and treatment for the histoplasmosis. I have looked into testing companies, but I simply cannot afford it. Any advice or assistance you could provide with testing would be very much appreciated. 2018/11/02 by privatge emailReply:
Watch out: the most important step for you to take with your daughter's illness is to be guided by advice from her doctors.
I found one research article (Patterson 1981) that related lung disease and fungi to sewage contamination indoors, focused on Cephalosporium.The histoplasmosis fungus is found throughout the world and grows in soil that has been enriched with bat or bird droppings or in bat droppings themselves. For example, the fungus is common around old chicken houses, in caves and other areas harboring bats, and around starling and blackbird roosts.
The fungus produces spores that can become airborne if the soil is disturbed. Inhalation of these spores may cause infection. - IDPH, Illinois department of health IDPH Chicago Headquarters Offices 122 S. Michigan Avenue, 7th and 20th Floors Chicago, IL 60603 312-814-2793 Retrieved 2018/11/10, original source: http://dph.illinois.gov/topics-services/diseases-and-conditions/diseases-a-z-list/histoplasmosis
HISTOPLASMOSIS FACT SHEET [PDF] Op. Cit. [Note that "sewage" as a pertinent vector for histoplasmosis-related illness is not mentioned in this article]However there are other respiratory illnesses that can be caused by, aggravated-by, or spread by sewage contamination in or around buildings, including the spread of harmful fungi or spores. Some research examples:
Cooke, William Bridge, and Paul Kabler. "ISOLATION OF POTENTIALLY PATHOGENIC FUNGI FROM POLLUTED WATER AND SEWAGE." [PDF] Public Health Reports 70, no. 7 (1955): 689. -full text PDF is also available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2024593/pdf/pubhealthreporig00163-0077.pdf
Patterson, Roy, Jordan N. Fink, Wayne B. Miles, John E. Basich, Donald B. Schleuter, David G. Tinkelman, and Mary Roberts. "Hypersensitivity lung disease presumptively due to Cephalosporium in homes contaminated by sewage flooding or by himidifier water." Journal of Allergy and Clinical Immunology 68, no. 2 (1981): 128-132.
Abstract:
Two cases of hypersensitivity lung disease apparently caused by home environment contamination with Cephalosporium have been identified. In one case repeated flooding of the home with sewer water appeared to be important in maintaining an environment contaminated with Cephalosporium and in the other case a contaminated humidfier appeared to be the source.
Both patients had chronic respiratory symptoms remitting during absence from the home, and both presented problems in diagnosis. In both cases cultures of the home environment or humidifier and serum antibody studies indicated Cephalosporium as the antigenic source responsible for the airway disease.
An inhalation challenge in one case was positive, adding further evidence for Cephalosporium as the antigenic source and etiologic agent. In both cases complete remission followed moving from the home. Cephalosporium is reported as an apparent antigenic source for home contamination resulting in significant chronic pulmonary morbidity.Also see
Contec®, CLEANING & DISINFECTING GUIDELINES FOR BIRD, BAT, AND RODENT DROPPINGS [PDF] Contec® Sporicidin® Contec, Inc. P.O. Box 530 Spartanburg, SC 29304 USA Tel: +1-864-503-8333 Toll Free US, Canada, PR: 1-800-289-5762 Email: info@contecinc.com
CLEANING UP AFTER RODENTS [PDF] U.S. CDC
- Hives
- hypersensitivity to airborne allergens or house dust
- hypersensitivity to mold
- Hypersensitivity Pneumonitis - (Extrinsic Allergic Alveolitis) - tightness of chest,
difficulty breathing,
cough, fever, muscle aches, reactions occur 6-8 hrs after exposure. - Uncommon
Hypersensitivity pneumonitis, associated with T-cell responses and responses mediated by immunoglobulin G (IgG). hypersensitivity pneumonitis is characterized by recurrent symptoms of fever, cough, and chest tightness and the presence of pulmonary infiltrates on a chest radiograph. Chronic hypersensitivity pneumonitis features progressive dyspnea, fatigue, interstitial pneumonitis, and pulmonary fibrosis (Farmer's lung)
Hypersensitivity pneumonitis is a rare immune system disorder that affects the lungs. It occurs in some people after they breathe in certain substances they encounter in the environment. These substances trigger their immune systems, causing short- or long-term inflammation, especially in a part of the lungs called the interstitium.
This inflammation makes it harder for the lungs to function properly and may even permanently damage the lungs. If diagnosed, some types of hypersensitivity pneumonitis are treatable by avoiding exposure to the environmental substances or with medicines such as corticosteroids that reduce inflammation.
If the condition goes untreated or is not well controlled over time, the chronic inflammation can cause irreversible scarring of the lungs that may severely impair their ability to function. - NIH, Hypersensitivity Pneumonitis, Also known as extrinsic allergic alveolitis, bird fancier’s lung, farmer’s lung, hot tub lung, and humidifier lung. Retrieved 2017/10/16, original source: https://www.nhlbi.nih.gov/health/health-topics/topics/hp
I
- Immune system deterioration, decreased resistance
- indigestion
- infertility
- Inflammatory bowel disease: Also see Chron's disease.
2019/04/09 The New York Times reported a possible relationship between abnormally high levels of presence of the fungus Malassezia in the intestines and both the presence of and possibly improved treatment for inflammatory bowel disease including Chron's disease. - Rogers, Lakeigh, "You're Covered in Fungi. How's Your Health? Researchers explore potential contributors to inflammatory bowel diseases." The New York Times, 9 April 2019, p. D-6. - Invasive pulmonary aspergillosis - pneumonia, fever, bone pain, chills - occurs in immunocompromised patients - uncommon. See ASPERGILLOSIS
- irritation: aggravated existing allergic rhinitis or asthma
- irritability
- irritable bowel syndrome
- itching skin, eye, nose, mouth
For skin-related itch and fiber complaints see your doctor. In addition to consulting your doctor who may in turn decide to refer you to a dermatologist, you might also benefit from reviewing the ITCHING & SCRATCHING RESEARCH found in our article concerning MORGELLONS SYNDROME.
Also see itching related to FIBERGLASS HAZARDS.
J
- judgment, loss of ability to think clearly and make decisions
K
- kidney pain and failure
L
- learning difficulties
- leaky gut syndrome
- liver pain
- long lasting flu-like symptoms
M
- Memory loss
- Menopause, unanticipated onset
- Metallic taste in mouth
- Migraine headaches
- Mood swings, sudden
- Morgellon's syndrome or Morgellon's disease: symptoms including
fibers in
nasal secretions, perceived
fibers in skin and scalp particles or scrapings -
skin lesions.
According to the Mayo Clinic Staff,
Morgellons disease is a mysterious skin disorder characterized by disfiguring sores and crawling sensations on and under the skin.
Although Morgellons disease isn't widely recognized as a medical diagnosis, experts from the Centers for Disease Control and Prevention (CDC) are investigating reports of the condition, which they refer to as unexplained dermopathy.
... Morgellons disease shares characteristics with various recognized conditions, including Lyme disease, liver or kidney disease, schizophrenia, drug or alcohol abuse, and a mental illness involving false beliefs about infestation by parasites (delusional parasitosis - Mayo Clinic
Please see this separate article: MORGELLONS SYNDROME
Note: OPINION-DF: various indoor environmental contaminants may in some cases be associated with skin irritation complaints, including exposure of insulation workers to high levels of contact with fiberglass insulation. In our experience skin irritation from fiberglass insulation generally diminishes rapidly and stops within 24-48 hours of bathing and thorough washing of dusty clothing.
Also see FIBERGLASS HAZARDS
Also see ITCHY FABRICS, FURNITURE and see ITCHING & SCRATCHING RESEARCH. - Mucous accumulation on back of the throat
- Multiple chemical sensitivity (MCS)
- Mycosis - various mycoses ascribed to mold exposure.
Watch out : some of these fungal infections can be very serious, even fatal, if not properly diagnosed and treated.- Aspergillosis: see ASPERGILLOSIS for details
- Blastomycosis: "blasto" most-common in the U.S. in the Ohio and Mississippi river valleys, as far north as Minnesota. Can infect humans, causing both lung and skin infections infections ranging from asymptomatic to very serious
- Candidiasis
- Coccidioidmycosis: "cocci", most-common in Southwestern U.S. to California, West Texas to SOCAL, soil fungi infecting animals, can infect humans, causing both lung and skin infections ranging from asymptomatic to very serious
- Cryptococcosis
- Histoplasmosis
- Hyphomycosis
- Mucormycosis
- Paracoccidiomycosis
- Phycomycosis
- Sporotrichosis
- Tinea / Ringworm
- Zygomycosis
- also see Trichothecene poisoning (below)
- Mycotoxicosis - Mycotoxins, which typically are cytotoxic, disrupt cell membranes and interfere with the synthesis of protein, RNA, and DNA The only well-documented human mycotoxicoses have been the result of ingestion rather than inhalation
- also see Trichothecene poisoning (below)
N
- Nasal discharge, green slime, fungus, mucous, other (See Morgellon's syndrome or Morgellon's disease above)
neck boils or round rash spots (see online photos) - night sweats and hot flashes
- nose irritation
- nosebleeds
- numbness in face and limb
O
- odors, increased sensitivity to, See ODOR DIAGNOSIS CHECKLIST, PROCEDURE
- Pungent odors may initiate avoidance reactions, a generalized feeling of discomfort, breath holding, and a burning sensation on the skin
- Open skin sores and lacerations
- open sores on head
- organic dust toxic syndrome
P
- Paracoccidiomycosis
Paracoccidioidomycosis is an endemic fungal disease acquired exclusively in Latin American countries, and that presents a greater prevalence in South America. Its etiological agent is the dimorphic fungus Paracoccidioides brasiliensis, which causes an infection that may progress to systemic granulomatous disease with tegumentary and visceral disease.
P. lutzii is another species recently identified within the genus Paracoccidioides, whose endemic area involves the Midwest and North regions of Brazil58. The characteristics of the disease caused by P. lutzii are still poorly known and therefore its epidemiology will not be considered in the present review.
Natural infection with P. brasiliensis occurs in men and animals and is acquired by the respiratory route after inhalation of fungal conidia suspended in air. Epidemiological surveys have permitted to estimate that many people have been infected with P. brasiliensis without developing the mycosis.
This condition is known as paracoccidioidomycosis-infection, in which the presence of the latent fungus in residual lung lesions and mediastinal lymph nodes is possible. Transmission of the disease through the skin or the mucosa is unlikely due to the low number of fungal propagules inoculated subcutaneously in small traumas.
A case of accidental percutaneous inoculation in the laboratory only caused a local granulomatous reaction18. There is no evidence of human transmission of paracoccidioidomycosis.
Paracoccidioidomycosis disease manifests as two main clinical forms that are epidemiologically distinct.
The acute/subacute form commonly affects children and young adults who tend to show more disseminated lesions. This form of the mycosis is assumed to appear a few weeks or months after infection with P. brasiliensis and therefore such cases, especially those involving children, are indicators of endemic areas of paracoccidioidomycosis77.
The chronic form of the disease is more common among adult men who present lesions usually involving the oral mucosa, the airways and the lungs. This form of the disease manifests months to years after P. brasiliensis infection and has been associated with specific risk factors.
Paracoccidioidomycosis has a great medical and social impact in the areas of higher endemicity, not only because of the considerable number of cases, but also because of the chronicity of the disease, the long duration of treatment and the frequent sequelae that cause inability to work and poor quality of life.
Among the causes of chronic granulomatous infectious diseases in Brazil, paracoccidioidomycosis is less frequent than tuberculosis, but is more common than histoplasmosis. Conversely, opportunistic histoplasmosis occurring in AIDS and other types of immunosuppression is more frequent than paracoccidioidomycosis. - Source: Martinez, Roberto. "Epidemiology of paracoccidioidomycosis." Revista do Instituto de Medicina Tropical de São Paulo 57 (2015): 11-20. retrieved 2017/10/16 - Peripheral nervous system effects
- personality changes
- pets, sudden odd behavior, aggressiveness, disorientation, running in circles,
stumbling, falling, respiratory disorder, sudden death, incl8uding death of pets due to pulmonary hemorraging [area of ongoing research by DJF - web author]
See: circling disease in sheep. See "The Toxic Effects of Mycotoxins on Humans, Sheep, & Possibly on Pets" discussed at MOLD EXPOSURE STANDARDS - Pets, Cryptococcosis of Cats; pet fatalities including pulmonary hemorrhaging, aberrant pet behavior similar to circling disease in sheep
- poor appetite
- puffy or droopy eyes
- Pulmonary hemorrhaging:
Comments & OPINION on certain health risks associated with Stachybotrys chartarum - a specific "black mold"
Stachybotrys chartarum (S. atra) is a large sticky spore not easily made airborne. Stachybotrys mycotoxin was thought to cause acute pulmonary hemorrhage and death in infants, but the CDC has stated that the association has not been proved).
About 10 ng of mycotoxins are produced for every 1 million mold spores [Probably widely variable from zero to high numbers based on environmental variables as well as species variation--DF].
Assuming the mold exposure effect is cumulative, inhalation of 109 spores per hour would be required for toxic effects. This is a very low level and easily obtained in circumstances where occupants are exposed to moldy building materials during demolition or cleaning. We investigated a report of death of a large dog who breathed high levels of Stachybotrys-chartarum-contaminated air during a demoltion project.
The dog's owner informed us that the dog's veternarian reported that the animal died of acute pulmonary hemorrhage. [4] However the most common effect of high levels of exposure to this black mold among our clients has been the onset of a skin rash. We also have fielded reports of neurological effects of exposure to mycotoxins including where this fungus was present.
Therefore, [in the opinion of some experts--DF] it is unlikely that inhalation of fungal parts presumed to contain mycotoxins could produce significant human illness--particularly in a nonagricultural setting.
QR
- Rashes - see Dermatitis (above) & Skin Rashes (below) and at FAQs at the end of this article.
- redness of eyes
- respiratory distress
- Rhinitis
- Ringing in ears
- Ringworm - see Tinea
- Runny nose
S
- Seizures [Obseved also in animals/pets - DF]
- smells, increased sensitivity to
- spleen pain
- shortness of breath (see Asthma, COPD, respiratory disorders)
- sinus congestion
- Sinusitis, cronic
- Skin rashes or irritation (example of a mold-complaint-related skin rash is shown at left)
also see DERMATITIS above and
our MOLD RELATED ILLNESS FAQs below for more photographs of skin rashes reported by clients who associated the rash onset with mold exposure.
Note that skin rashes can be caused by a very long list of environmental and health conditions, and some of these may not be obvious.
For example, in the U.S. the browntaiul moth caterpillar (Euproctis chrysorrhoea) [photo below], endemic in Maine, sport poisonous hairs that can remain toxic for up to three years and can cause a red bumpy rash that looks like poison ivy.
- skin redness
- sleep disorders
See the Q&A on "Sleep Apathy" found at MOLD RELATED ILLNESS FAQs-2 - slurred speech or verbal dysfunction (trouble in speaking)
- sneezing fits
- spitting up or vomiting mucous
- Sporotrichosis
Summary: Sporotrichosis, which is caused by the dimorphic fungus Sporothrix schenckii, is currently distributed throughout the world, especially in tropical and subtropical zones. Infection generally occurs by traumatic inoculation of soil, plants, and organic matter contaminated with the fungus. Certain leisure and occupational activities, such as floriculture, agriculture, mining, and wood exploitation, are traditionally associated with the mycosis.
Zoonotic transmission has been described in isolated cases or in small outbreaks. Since the end of the 1990s there has been an epidemic of sporotrichosis associated with transmission by cats in Rio de Janeiro, Brazil. More than 2,000 human cases and 3,000 animal cases have been reported. In humans, the lesions are usually restricted to the skin, subcutaneous cellular tissue, and adjacent lymphatic vessels.
In cats, the disease can evolve with severe clinical manifestations and frequent systemic involvement.
The gold standard for sporotrichosis diagnosis is culture. However, serological, histopathological, and molecular approaches have been recently adopted as auxiliary tools for the diagnosis of this mycotic infection. The first-choice treatment for both humans and cats is itraconazole. -
Source: de Lima Barros, Mônica Bastos, Rodrigo de Almeida Paes, and Armando Oliveira Schubach. "Sporothrix schenckii and Sporotrichosis." Clinical microbiology reviews 24, no. 4 (2011): 633-654.
- swollen glands
- swollen lymph nodes
- Syndromes, mold-related
- Otomycosis
- Phaeohyphomycosis
- Rhinosporidiosis
- Systemic candida infection - see Candida
T
- Throat irritation
- Tightness in the chest (this can be a common symptom of many complaints including mold-triggered asthma attacks)
- Tinea (Ringworm) most common fungal disease is this superficial mycosis, not linked to IAQ/building-related illness. Highly contaigous.
Ringworm is a common skin infection that is caused by a fungus. It's called "ringworm" because it can cause a circular rash (shaped like a ring) that is usually red and itchy.
Anyone can get ringworm. The fungi that cause this infection can live on skin, surfaces, and on household items such as clothing, towels, and bedding. Ringworm goes by many names. The medical terms are "tinea" or "dermatophytosis."
Other names for ringworm are based on its location on the body — for example, ringworm on the feet is also called "athlete's foot. - NIH, About Ringworm, retrieved 2017/10/16 original source: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024876/
Also see this ringworm information at the US CDC - https://www.cdc.gov/fungal/diseases/ringworm/index.html
Tinea versicolor, also referred to as pityriasis versicolor, is a skin condition characterized by small patches of lighter or darker skin. It is caused by a type of fungus that is found on almost everyone’s skin. It is generally not harmful and it isn't contagious.
Topical treatments, such as special creams or shampoos, are usually effective.
Symptoms of Tinea Versicolor
In tinea versicolor, small round or oval patches of skin appear at first, and later merge into larger patches with irregular shapes. They are especially common on the back, chest, neck and/or arms. They may occur on the face as well, particularly in children.
The patches may be yellow or brownish, or sometimes red or pink. They are usually lighter or darker than the surrounding healthy skin. Because these patches hardly change color in the sun, they are more noticeable if you have a suntan. But if you have a fair complexion, they may turn a little brownish. The affected areas of skin may also be somewhat scaly. They rarely itch. If they do, then they only itch a little. - NIH Tinea versicolor, retrieved 2017/10/16, original source: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0076676/
- Tremors (shaking)
Trichothecene mycotoxin poisoning symptoms & medical research
- Trichothecene poisoning (Alternate names: Mycotoxins, T2, Yellow rain) - possibly related to mycotoxin exposure from some molds.
The US CDC offers lab criteria for diagnosis of Trichothecend poisoning including:- Biologic: Selected commercial laboratories are offering immunoassays to identify trichothecenes or trichothecene-specific antibodies in human blood or urine (2, 3). However, these procedures have not been analytically validated and are not recommended.
- Environmental: Detection of trichothecene mycotoxins in environmental samples, as determined by FDA.
- References for poisoning by mycotoxins, T2, Yellow Rain, or Trichothecenes:
Clinical Guide to Bioweapons and Chemical Agents, Vincent E. Friedewald, Springer, London, ISBN 978-1-84628-787-9 (online),
Trichothecene poisoning is discussed in depth at the US CDC website where the following references are also provided: - Wannemacher RW Jr, Wiener SL. Trichothecene mycotoxins. In: Zajtchuk R, Bellamy RF, eds. Textbook of military medicine: medical aspects of chemical and biologic warfare. Washington, DC: Office of the Surgeon General at TMM Publications, Borden Institute, Walter Reed Army Medical Center; 1997:655-77.
- Croft WA, Jastromski BM, Croft AL, Peters HA. Clinical confirmation of trichothecene mycotoxicosis in patient urine. J Environ Biol 2002;23:301-20.
- Vojdani A, Thrasher HD, Madison RA, Gray MR, Heuser G, Campbell AW. Antibodies to molds and satratoxin in individuals exposed in water-damaged buildings. Arch Environ Health. 2003;58:421-32.
- Tuomi T, Reijula K, Johnsson T, et al. Mycotoxins in crude building materials from water-damaged buildings. Appl Environ Microbiol 2000;66:1899-904.
- US CDC: "Case Definition: Trichothecene Mycotoxin", http://www.bt.cdc.gov/agent/trichothecene/casedef.asp 3/30/09 discusses the possibility of making weapons from Trichothecene mycotoxins.
Reader follow-up:
2016/11/12, Anna levis said:
The trichothecene mycotoxins produced by toxic black mold are neurotoxic. This means they can kill neurons in the brain and impair a person’s mental ability. They also cause nervous disorders such as tremors and can cause personality changes such as mood swings and irritability.
Symptoms of trichothecene mycotoxin poisoning:
- Aggression and other personality changes - we have observed this first-hand and also call readers' attention to sheep circling disease - Ed.
- Anxiety
- Brain fog
- Confusion
- Depression
- Difficulty concentrating and paying attention
- Disorientation
- Dizziness
- Hallucinations
- Impaired learning ability
- Memory loss and memory problems
- Numbness
- Seizure
- Shaking
- Shock
- Shortened attention span
- Slowed reflexes
- Tingling
- Trembling
This comment was posted originally
at MOLD CLEANUP - WOOD FRAMING & PLYWOOD
Thanks, Anna,
The phrase "black mold" is very misleading.
- First, not all "black molds" are toxic and that there are plenty of molds of other colors that are equally risky or health-hazards for people. See BLACK COSMETIC MOLD - not all black mold is harmful
- Second, of the millions+ genera/species of molds found on earth, or even just the few hundred commonly-found in buildings, there are many mold genera/species that are not black, may be light colored, even white or light green or gray and that as harmful or even a greater health risk that the most-popular "toxic black mold" of Stachybotrys chartarum.
For example the very small and often pathogenic Aspergillus or Penicillium mold spores are very common in buildings and probably cause far more illnesses than S. chartarum. We report and we blame what's easy to see, not necessarily what's present and most harmful.
S. chartarum is a comparatively large sticky spore that is not easily airborne, as much as 25 times larger than an Aspergillus or Penicillium mold spore. Aspergillus or Penicillium mold spores are easily airborne and can remain in the air for many hours, moving in a building more or less as would a gas riding on air currents. - Third, Watch out: the symptoms you listed... that you quoted from a website, are absolutely not restricted to trichothecene mycotoxin poisoning and could be caused by any of a large number of conditions, hazardous exposures, or by other health problems. People suffering from the symptoms you listed should consult with their doctor promptly and in extreme cases should seek immediate emergency medical care.
Research on trichothecene mycotoxin poisoning
- MOLD ATLAS & PARTICLES INDEX - Index & photo-guide to indoor mold, pathogens, allergens, particles . Medical Health Effects of Mold, House Dust. Health Effects of Fiberglass, Animal Dander, Insect Fragments, Etc. Photographs of building mold are in this document
- Rocha, O., K. Ansari, and F. M. Doohan. "Effects of trichothecene mycotoxins on eukaryotic cells: a review." Food additives and contaminants 22, no. 4 (2005): 369-378.
- Sorenson, W. G., DAVID G. Frazer, BRUCE B. Jarvis, J. A. N. E. T. Simpson, and V. A. Robinson. "Trichothecene mycotoxins in aerosolized conidia of Stachybotrys atra." Applied and Environmental Microbiology 53, no. 6 (1987): 1370-1375.
- Ueno, Y., N. Sato, K. Ishii, K. Sakai, H. Tsunoda, and M. Enomoto. "Biological and chemical detection of trichothecene mycotoxins of Fusarium species." Applied microbiology 25, no. 4 (1973): 699.
- Krska, R., S. Baumgartner, and R. Josephs. "The state-of-the-art in the analysis of type-A and-B trichothecene mycotoxins in cereals." Fresenius' journal of analytical chemistry 371, no. 3 (2001): 285-299.
- Yang, Gi-Hyeok, Bruce B. Jarvis, Yong-Joo Chung, and James J. Pestka. "Apoptosis induction by the satratoxins and other trichothecene mycotoxins: relationship to ERK, p38 MAPK, and SAPK/JNK activation." Toxicology and applied pharmacology 164, no. 2 (2000): 149-160.
- Smoragiewicz, Wanda, Bruno Cossette, Armel Boutard, and Krzysztof Krzystyniak. "Trichothecene mycotoxins in the dust of ventilation systems in office buildings." International archives of occupational and environmental health 65, no. 2 (1993): 113-117.
- Wannemacher, Robert W., STANLEY L. Wiener, Frederick R. Sidell, Ernest T. Takafuji, and David R. Franz. "Trichothecene mycotoxins." Medical aspects of chemical and biological warfare (1997): 655-676.
U
- unexplained fevers
- Upper respiratory symptoms (eg, nasal congestion, sinus headache, episodic dyspnea)
- urinary tract infection (UTI)
V
- Vaginal yeast infections - wee Women' health problems (below)
- vertigo or dizziness
- VOC sensitivity:
- volatile organic chemicals may reach levels sufficient to produce central nervous system symptoms such as headache, inability to concentrate, or dizziness
- vomiting (nausea)
WXYZ
- Weakness, loss of strength
- wheezing breath
- women's health problems, nonspecific
- yeast infections, vaginal, (other?) symptoms: Vaginal. Recurrent episodes of Candida vaginitis associated with the classic symptoms of pruritus, burning and abnormal discharge.
- Gastrointestinal. Heartburn, bloating, diarrhea or constipation.
- Respiratory allergy. Rhinitis, sneezing and/or wheezing.
- Central nervous system. Anxiety, depression, memory deficits and/or loss of ability to
concentrate. - Menstrual abnormalities. Severe premenstrual tension and/or menstrual irregularities.
Other Systemic Symptoms. - Fatigue, headache and/or irritability.
- Zygomycosis, mucormycosis or phycomycosis or hyphomycosis
Zygomycosis, also known as mucormycosis or phycomycosis or hyphomycosis, is a rapidly-progressive life-threatening deep fungal infection primarily affecting patients with decreased immunity.
Rare compared to other infectious pathologies, it is gaining more ground recently. Mucormycosis has predilection for certain groups of people, including immune-suppressed and diabetic patients.
This aggressive infection comes in a variety of forms. Despite recent advances in its medical and surgical treatments, it still retains a poor prognosis with high morbidity and mortality.
...
Mucormycosis is a broad term for a multitude of diseases caused by infection with different fungi in the order of Mucorales. The most common causative organisms are from the Rhizopus species.
Other species include, in descending order, include Rhizomucor, Cunninghamella, Apophysomyces, Saksenaea, Absidia, Mucor, Syncephalastrum, Cokeromyces, and Mortierella.[1] These fungi are ubiquitous in nature and have world-wide distribution. Mucor is a rapidly growing fungus that is usually dark gray or light olive gray when grown on typical laboratory media.
It is easily recognizable microscopically by its tall needle like sporangiophores and large sporangium. The mold grows and spreads quickly. Like other members of the class Zygomycetes, Mucor fungi can reproduce asexually with spores, or sexually by fusing to create zygospores which contain a mixture of genetic material. Mucor can be present in the outdoor or indoor settings. In the outdoors, it can be found in soil, decaying vegetation, hay, stored seeds or horse manure. Indoors, it can be found in house dust, and poorly maintained vacuum systems or dirty carpets.
One study looking at the most frequent molds found in house dust found Mucor in 98% of the samples from homes in Denmark and 31% of the samples in homes in Canada.[2] Heavy inhalation of the Mucor spores can cause extrinsic allergic alveolitis and ultimately pulmonary fibrosis if the fungus exposure persists.
The supreme danger of Mucor, however, lays in the fact that it can become an opportunistic pathogen causing deep fungal infection when conditions are right. Ripe conditions for aggressive zygomycosis include significantly compromised immunity such in malignancy, neutropenia, use of immunosuppressive agents, metabolic acidosis, uncontrolled diabetes, starvation, severe trauma or other forms of debilitation. It is well documented that they can cause a multitude of pathologies not only in humans but also in cattle, sheep, swine and dogs.[3]
In Australia, mucormycosis was documented to cause severe skin lesions in frogs[4] and the Tasmanian platypus.[5] The histopathologic hallmark of this infection is the mycotic invasion of the blood vessels, often leading to thrombosis, followed by tissue infarction and necrosis mediated by fungal proteases, lipases and mycotoxins.[6] This aggressive vasculature invasion can not only affect the small vessels such as arterioles but can also reach large arteries causing devastating results such as rupture of the aorta.[7]
- The Rise of an Oppurtunistic Infection called “Invasive Zygomycosis” Abdelkarim Waness, Ghuzayel Al Dawsari, and Hamdan Al Jahdali at US NIH https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2840956/
Watch Out: this MOLD RELATED ILLNESS SYMPTOMS list is a complaint list, not a medical document. It has not been peer-reviewed by the medical profession, and this list is not in any medical sense authoritative, nor can any list of mold illness complaints or symptms be complete. Readers can not rely on this document for medical diagnosis and instead should consult with their physician or with a specialist such as a medical toxicologist.
...
Reader Comments, Questions & Answers About The Article Above
Below you will find questions and answers previously posted on this page at its page bottom reader comment box.
Reader Q&A - also see RECOMMENDED ARTICLES & FAQs
On 2020-08-10 - by (mod) -
 Not sure, Micah, but clearly there's water damage and falling plaster; I see what looks like rusty debris from metal or wood - the photo lacks context.
Not sure, Micah, but clearly there's water damage and falling plaster; I see what looks like rusty debris from metal or wood - the photo lacks context.
On 2020-08-10 by Micah
What am I looking at? It's inside the walls of my bathroom
On 2020-06-29 - by (mod) -
Gina
You should take these questions to your doctor, someone who can examine and interview you in detail and with the proper expertise. On internet there are just too many opinions without diagnosis.
It's reasonable then, to ask your doctor about the plausible causes of your complaints and symptoms, including of course contaminants in the indoor environment.
On 2020-06-29 by Gina
My boyfriend and I have been living in an apartment that had a huge leak from the kitchen that extended to the living room carpet n thru bathroom wall. We are now seeing black discoloration under our skin, black ooze from our skin along with other issues.
We know mold us in our apt as it's in every window seal n overtaking one bedroom which we do not use. Of course other symptoms with dizziness n chills etc but is the discoloration probably due to over exposure of mold spores?
On 2020-06-23 by (mod) - moldy sippy cup hazards?
Jamie
That doesn't sound like a mold problem to me, but nobody can diagnose illnesses by a brief e-text; I'd say if the problem persists check with your doctor.
On 2020-06-23 by Jamie
I used a sipping cup yesterday that I haven't used in about 2 months. The last time it was used was for storing prepped scrambled eggs.
I used it for my iced coffee this time. I was having a hard time drinking out of the sipper spout, when I got a big release, a big sliver of fungus like hard substance came out! Ever since, I have a weird dry patch in the back of my throat. Is this something to be worried about?
On 2020-05-25 - by (mod) -
 Sorry, Layla but no, not from your photo alone can one identify that the material is mold nor, if it is mold, what's the genera/species.
Sorry, Layla but no, not from your photo alone can one identify that the material is mold nor, if it is mold, what's the genera/species.
That looks to me like efflorescence and moisture leaks through a plaster wall.
The amount looks trivial - clean up using normal household cleaners; watch for signs of and investigate further if there are leaks into the wall.
On 2020-05-25 by Layla
Any idea what kind of mold?
On 2020-01-18 by (mod) - Can mold inter your body thru the skin?
No, Mitzi, in general mold, that is mold spores, cannot enter your body directly through your skin unless the skin is cut or similarly compromised.
However
- mold spores of SOME molds (not all molds are pathogenic or harmful to humans) can get into an open cut or sore on your body to possibly cause a fungal infection there.
- some mold spores can get into a sinus cavity through being inhaled through the nose to give a fungal sinus infection
- some small mold spores such as members of the Aspergillus or Penicillium mold families can be breathed into the lung and in immune-compromised people can lead to fungal infection there - such as Aspergillosis
- And finally, WHILE THE HEALTH RISK IS LOW For MOST PEOPLE (Boonen 2012) it might be possible for MYCOTOXINS in a few molds including MVOCs to be absorbed through the skin
- that's not spores entering the body but rather chemicals produced by some molds.
See
Boonen, Jente, Svetlana V. Malysheva, Lien Taevernier, José Diana Di Mavungu, Sarah De Saeger, and Bart De Spiegeleer. "Human skin penetration of selected model mycotoxins." Toxicology 301, no. 1-3 (2012): 21-32.
Abstract:
Dermal exposure data for mycotoxins are very scarce and fragmentary, despite their widespread skin contact and hazard toxicity. In this study, the transdermal kinetics of aflatoxin B1 (AFB1), ochratoxin A (OTA), fumonisin B1 (FB1), citrinin (CIT), zearalenone (ZEA) and T-2 toxin (T-2) were quantitatively evaluated, using human skin in an in vitro Franz diffusion cell set-up.
All mycotoxins penetrated through the skin, except for FB1, which showed concentrations in the receptor fluid below the LoD, resulting in a Kp < 3.24 × 10−6 cm/h. ota showed the highest permeation (kp = 8.20 × 10−4 cm/h), followed by cit (kp = 4.67 × 10−4 cm/h). afb1 and zea showed lower permeability rates (kp = 2.11 and 2.33 × 10−4 cm/h, respectively).
t-2 was found to have the lowest permeability (kp = 6.07 × 10−5 cm/h). from literature-based mycotoxin-concentrations, dermal contact surface, exposure time and apparent kp's obtained in this study, the daily dermal exposure (dde) in two industrial and one residential scenario was estimated. dermal exposure to the dna-reactive genotoxic carcinogenic afb1 can lead to a health risk for agricultural workers which are exposed to a mycotoxin contaminated solution in a worst case situation.
for all the other investigated mycotoxins, no significant health risk is calculated after dermal contact in neither agricultural nor residential environments.
kemppainen, b. w., r. t. riley, and j. g. pace. "skin absorption as a route of exposure for aflatoxin and trichothecenes." journal of toxicology: toxin reviews 7, no. 2 (1988): 95-120.
senkpiel, k., d. sassenberg, r. keller, and h. ohgke. "content of mycotoxins in conidiospores from mould in buildings." mycotoxin research 16, no. 1 (2000): 88-93.>
On 2020-01-18 by Mitzi
Can mold inter your body thru the skin?
...
Continue reading at MOLD RELATED ILLNESS GUIDE or select a topic from the closely-related articles below, or see the complete ARTICLE INDEX.
Or see MOLD RELATED ILLNESS FAQs - questions & answers posted originally at this article
Or see these
Recommended Articles
- BLACK MOLD, HARMLESS - Photos of of often recognizable, usually harmless or cosmetic black mold on wood
- MOLD APPEARANCE - WHAT MOLD LOOKS LIKE - Photos of what mold looks like in buildings, organized by mold color and appearance.
- MOLD APPEARANCE - STUFF THAT IS NOT MOLD - Photos of material that is not mold but is sometimes mistaken for mold
- MOLD ATLAS & PARTICLES INDEX, Pathogens, Allergens and Other Indoor Particles - actual and possible medical health effects of Mold (separate online document)
- MOLD CLEANUP GUIDE- HOW TO GET RID OF MOLD
- MOLD DOCTORS - ENVIRONMENTAL MEDICINE
- MOLD EXPOSURE STANDARDS
- MOLD FREQUENCY in BUILDINGS - Table of what mold genera/species are frequently found in indoor mold tests.
- MOLD GROWTH ON SURFACES, PHOTOS - Photos of what mold looks like in buildings on more than 100 surfaces, organized by mold growth on various kinds of building surfaces and contents or items found in buildings. Mold in situ.
- MOLD GROWTH on SURFACES, TABLE OF - Summary table of what mold genera/species are frequently found on various building surfaces and materials
- MOLD BY MICROSCOPE - Mold under the microscope - photo identification of the most common indoor molds found in buildings
- MOLD in the PETRI DISH, PHOTOS - what mold looks like on culture plates or in culture-type mold test kits
- MOLD RELATED ILLNESS GUIDE
- MOLD RELATED ILLNESS SYMPTOMS
- MOLD SPORES in the HOME - a Photo ID Library for detection and identification of mold allergens on indoor building surfaces and for an atlas of building molds.
- WHO MOLD BULLETIN
Suggested citation for this web page
MOLD RELATED ILLNESS SYMPTOMS at InspectApedia.com - online encyclopedia of building & environmental inspection, testing, diagnosis, repair, & problem prevention advice.
Or see this
INDEX to RELATED ARTICLES: ARTICLE INDEX to MOLD CONTAMINATION & REMEDIATION
Or use the SEARCH BOX found below to Ask a Question or Search InspectApedia
Ask a Question or Search InspectApedia
Questions & answers or comments about possible symptoms of mold related illness & health complaints.
Try the search box just below, or if you prefer, post a question or comment in the Comments box below and we will respond promptly.
Search the InspectApedia website
Note: appearance of your Comment below may be delayed: if your comment contains an image, photograph, web link, or text that looks to the software as if it might be a web link, your posting will appear after it has been approved by a moderator. Apologies for the delay.
Only one image can be added per comment but you can post as many comments, and therefore images, as you like.
You will not receive a notification when a response to your question has been posted.
Please bookmark this page to make it easy for you to check back for our response.
IF above you see "Comment Form is loading comments..." then COMMENT BOX - countable.ca / bawkbox.com IS NOT WORKING.
In any case you are welcome to send an email directly to us at InspectApedia.com at editor@inspectApedia.com
We'll reply to you directly. Please help us help you by noting, in your email, the URL of the InspectApedia page where you wanted to comment.
Citations & References
In addition to any citations in the article above, a full list is available on request.
- [1] "Damp house linked to kids' risk of nasal allergies", New York Times, 1 Aug 2010 (Reuters Health). The New York Times reported that "Children who live in damp, water-damaged homes may be more likely than other kids to develop nasla allergies, a new study suggests." The Finnish study of 1,900 children over a six year period found that 16 percent of damp-home children were diagnosed with allergic rhinitis over the next 6 years compared with just under 12 percent of children whose parents reported no dampness problems. [NOTE: our field and lab experience indicate that homeowners are not accurate in reporting the presence of mold and dampness problems except when conditions are sufficiently severe that there is ample visible or odor evidence of mold or other contaminants.-DF]
- [2] "Home Dampness and Molds as Determinants of Allergic Rhinitis in Childhood: A 6-Year, Population-based Cohort Study",
Jouni J. K. Jaakkola*, Bing-Fang Hwang and Maritta S. Jaakkola,
* Correspondence to Dr. Jouni J. K. Jaakkola, Institute of Health Sciences, Aapistie 1, P.O. Box 5000, 90014 Oulu, Finland (e-mail: jouni.jaakkola@oulu.fi),
Accepted for publication April 8, 2010.,
The authors assessed the relation between exposure to dampness and molds in dwellings and the development of allergic rhinitis in childhood in a 6-year, population-based prospective cohort study of 1,863 children aged 1–7 years at baseline in 1991 (follow-up rate, 77%) from Espoo, Finland. The studied exposures were history of water damage, presence of moisture and visible mold, and perceived mold odor in the home, based on parent-administered questionnaire. A total of 246 (13.2%) children developed physician-diagnosed allergic rhinitis during the study period, resulting in an incidence rate of 440 cases per 10,000 person-years (95% confidence interval (CI): 387, 499). In logistic regression adjusting for confounding, any mold or dampness exposure indicator at baseline (adjusted odds ratio = 1.55, 95% CI: 1.10, 2.18), at follow-up (adjusted odds ratio = 1.62, 95% CI: 1.21, 2.18), or both (adjusted odds ratio = 1.96, 95% CI: 1.29, 2.98) was an important independent determinant of the risk of allergic rhinitis. Of the individual indicators, water damage and moisture on the surfaces were consistent determinants of allergic rhinitis. The results of this cohort study, which assessed exposure before the onset of allergic rhinitis, strengthen considerably the evidence of the role of indoor dampness problems as determinants of allergic rhinitis in children.
Keywords: air pollution, indoor; fungi; housing; rhinitis, allergic, perennial
American Journal of Epidemiology Advance Access published online on July 16, 2010
American Journal of Epidemiology, doi:10.1093/aje/kwq110
Oxford University Press
The American Journal of Epidemiology is the premier epidemiological journal devoted to the publication of empirical research findings, methodological developments in the field of epidemiological research and opinion pieces. It is aimed at both fellow epidemiologists and those who use epidemiological data, including public health workers and clinicians. ISSN: 1476-6256 - [3] "Morgellons disease: managing a mysterious skin condition", The Mayo Clinic, web search 02/27/2011, original source: http://www.mayoclinic.com/health/morgellons-disease/sn00043
- [4] P.I. "Onsite Mold Investigation including sick individuals, sick pets, skin rashes, death of one pe", Daniel Friedman, 6/1/2004, private investigation report, lab work, site photos, on file.
- Identifying Filamentous Fungi, A Clinical Laboratory Handbook, Guy St-Germain, Richard Summerbell, Star Publishing, 1996, ISBN 0-89863-177-7 (English)
- Fundamentals of Diagnostic Mycology, Fran Fisher, Norma B. Cook, W.B. Saunders Co. 1998, ISBN 0-7216-5006-6
- Atlas of Clinical Fungi, 2nd Ed., GS deHoog, J Guarro, J Gene, & MJ Figueras, Centraalbureau voor Schimmelcultures, Universitat Rovira I Virgili, 2000, ISBN 90-70351-43-9
- http://www.doctorfungus.org/ online mycology reference http://www.postgradmed.com/issues/2003/06_03/fung.htm
- http://www.cleanwaterpartners.org/mold/related-illnesses.html (Environmental Law Firm site)
- http://www.dhs.ca.gov/ohb/HESIS/molds.pdf California DHS "Molds in Indoor Workplaces"
- In addition to citations & references found in this article, see the research citations given at the end of the related articles found at our suggested
CONTINUE READING or RECOMMENDED ARTICLES.
- Carson, Dunlop & Associates Ltd., 120 Carlton Street Suite 407, Toronto ON M5A 4K2. Tel: (416) 964-9415 1-800-268-7070 Email: info@carsondunlop.com. Alan Carson is a past president of ASHI, the American Society of Home Inspectors.
Thanks to Alan Carson and Bob Dunlop, for permission for InspectAPedia to use text excerpts from The HOME REFERENCE BOOK - the Encyclopedia of Homes and to use illustrations from The ILLUSTRATED HOME .
Carson Dunlop Associates provides extensive home inspection education and report writing material. In gratitude we provide links to tsome Carson Dunlop Associates products and services.