Aspergillosis: basic information
Aspergillosis: basic information
Aspergillus-related disease & health complaints, inspecting buildings for Aspergillus mold contamination; treatment for Aspergillosis
- POST a QUESTION or COMMENT about Aspergillus & Aspergillus-related illnesses
Aspergillosis illnesses & Aspergillus mold in buildings:
This article provides basic descriptions of Aspergillus-related illnesses and discusses valid versus in-valid inspection and testing techniques used to detect mold contamination in buildings, including Aspergillus sp. molds.
At page top: an Aspergillus sp. conidiophores under the microscope at about 1200x.
InspectAPedia tolerates no conflicts of interest. We have no relationship with advertisers, products, or services discussed at this website.
- Daniel Friedman, Publisher/Editor/Author - See WHO ARE WE?
Aspergillus related illnesses & Aspergillus Contamination Testing in Buildings
There are approximately 180 species of Aspergillus, but fewer than 40 of them are known to cause infections in humans. Aspergillus fumigatus is the most common cause of human Aspergillus infections. Other common species include A. flavus, A. terreus, and A. niger. (U.S. CDC 2019)
Watch out: people who are concerned about possible mold-related illness should consult their primary care physician and with that doctor's advice decide if referral to a pulmonologist with expertise in mold related illness is appropriate.
We also issue this trigger warning: reading this material can cause an anxiety-induced asthma attach, though most likely if you read with care you'll see that for most people anxiety is merited.
Greenberger (2002) discusses allergic bronchopulmonary aspergillosis (ABPA) as an illness complicating asthma and cystic fibrosis, noting that The survival factors in Aspergillus fumigatus that support saprophytic growth in bronchial mucus are not understood.
At left: Aspergillus fumigatus conidiophore showing characteristic long spore chains - lab photo, Daniel Friedman.
[Click to enlarge any image]
Beyond asthmatics and people with cystic fibrosis, and focusing on immunie-impaired patients, Cornet (2002) notes that invasive aspergillosis is the most prevalent mould infection, and Soubani (2002) offers this recap of the importance of recognizing and treating pulmonary aspergillosis, particularly for people with a compromised immune system but as well for patients suffering from asthma:
Aspergillus is a ubiquitous fungus that causes a variety of clinical syndromes in the lung, ranging from aspergilloma in patients with lung cavities, to chronic necrotizing aspergillosis in those who are mildly immunocompromised or have chronic lung disease.
Invasive pulmonary aspergillosis (IPA) is a severe and commonly fatal disease that is seen in immunocompromised patients, while allergic bronchopulmonary aspergillosis is a hypersensitivity reaction to Aspergillus antigens that mainly affects patients with asthma.
In light of the increasing risk factors leading to IPA, such as organ transplantation and immunosuppressive therapy, and recent advances in the diagnosis and treatment of Aspergillus-related lung diseases, it is essential for clinicians to be familiar with the clinical presentation, diagnostic methods, and approach to management of the spectrum of pulmonary aspergillosis.
Patterson (2000) as well as virtually all authors writing in this field emphasize the importance of early diagnosis and treatment in the successful outcome for people with invasive aspergillosis while also noting that rapid diagnosis of invasive aspergillosis - a more serious illness - is difficult as most facilities lack the tools for definite diagnosis, making clinical detection of central importance.
By 2007 Greene described the use of computed tomography (CT) and the "halo sign" in diagnosing invasive pulmonary aspergillosis (IPA), concluding
Initiation of antifungal treatment on the basis of the identification of a halo sign by chest CT is associated with a significantly better response to treatment and improved survival.
[Click to enlarge any image]
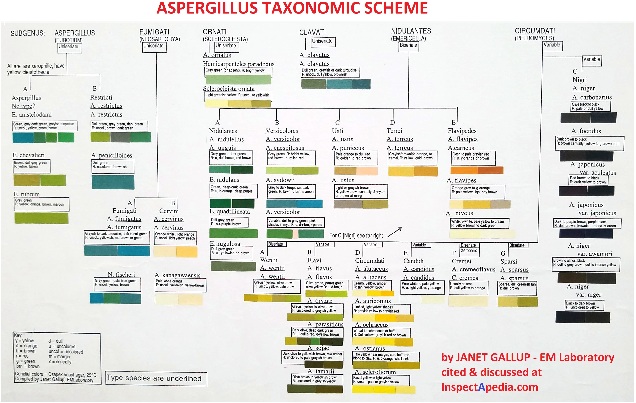
The Aspergillus Taxonomic Scheme generously provided above by Janet Gallup, EMLaboratory, shows that while there are light colors of species of Aspergillus, most of its species are more-exciting in their pigment.
Reader Question: what kind of home tests make sense for someone testing positive for Aspergillus fumigatus?
15 September 2015 Caroline said:
My father tested positive for Aspergillus fumigatus. I called some mold testing people to come out & all of them said they would do an air test in his room ( which is in the basement) and in the basement.
I read how you said an air quality test is not always accurate because of the changes in the room, so I was wondering what kind of testing you would recommend. Also, I do have a compost heap outside. So I wondered if I got rid of it, would it take care of the situation?
Reply:
Caroline,
You can find my email at the page bottom CONTACT link and by email I can offer a number for pro-bono consulting in this matter.
There is a place for air testing and properly done it can be informative. But considering the orders of magnitude variation in measurements of the level of airborne particles just in response to very small changes (waving a notebook in the air for example), a "negative" air test result cannot be trusted, and even a "positive" air test for mold that produces a high mold count cannot for a moment be presumed to actually describe the level of exposure of the building occupants to mold.
Recommended building Inspection & Test Procedures for Mold Contamination
And no “test for mold” alone is going to tell us where the problem is nor what needs to be done about it. It’s instead a profitable “indicator test” that might find evidence of a problem that’s really there - or it might miss a real problem. The physician needs to be included in the process.
An effective mold contamination investigation, to be useful, must be accurate and it must be prescriptive.
- Decide if a mold investigation is warranted.
See MOLD / ENVIRONMENTAL EXPERT, HIRE ? - A thorough client interview, case history, complaints, relationship of complaints to building, other occupants' experiences. If the client or person of concern has not yet done so she or he should see their doctor promptly. If you and your doctor need to look further for a specialist in environmental medicine
See MOLD DOCTORS - ENVIRONMENTAL MEDICINE - A thorough visual inspection of the building by an expert who understands building science, how air moves in building, how and where leaks occur, what building materials are mold friendly, how to decide when invasive inspection is justified (cutting openings to look into a wall where leaks have occurred, for example)
See MOLD INVESTIGATION PROCEDURE TIPS
and
See MOLD APPEARANCE - WHAT MOLD LOOKS LIKE
and
See HIDDEN MOLD, HOW TO FIND - Collection of a few intelligently-selected samples of settled building dust to be screened for unusual levels of harmful molds or even at very low levels, for clues suggesting a nearby Aspergillus contamination source (mold reservoir) such as the observation of Aspergillus spores in spore chains.
See MOLD TEST KIT INSTRUCTIONS - note: do not send mold samples to InspectApedia; select a qualified mold lab. - Air tests as a screen for mold: Optionally, I don't mind air testing as well, with the caveats I've already given. A negative air test result, taken alone, cannot be trusted.
See ACCURACY OF AIR TESTS for MOLD
and
See MOLD TEST PROCEDURES - An action plan: Identification of mold reservoirs in the building and if appropriate, an action plan for removing the mold and correcting its cause.
See MOLD CLEANUP GUIDE- HOW TO GET RID OF MOLD
and
See MOLD PREVENTION GUIDE - home
Watch out: opportunists of all levels of education and training have leapt enthusiastically into the "mold business"; but only a few do the real job. It is far too tempting, too profitable, and easier and faster to just stop by and "collect an air sample.
Even if the sample’s lab result says “yes there is a problem here” that alone is not diagnostic nor prescriptive. It doesn't tell us where the problem is (or where they are), what cleanup is needed, what corrections are needed to prevent future problems.
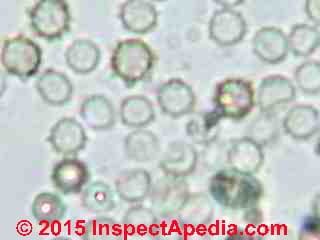
Aspergillus sp. mold spore photographs
The following is excerpted from MOLD by MICROSCOPE


Photographs of Aspergillus sp. mold spores under the microscope (above left) and Aspergillus niger culture (above right). Because their airborne spores look similar, also see Penicillium culture [image file], and also see these Penicillium spores [image file].
Aspergillus and Penicillium spores are difficult to differentiate when they are found in air that you may see them reported in test results as "Pen/Asp".
Watch out: Most Pen/Asp spores are round, hyaline (colorless) and small and lack surface features to aid in their precise identification by microscope when the spores are found alone, or in air samples (and if not in spore chains). In that case the spores may not even be identified as (potentially harmful) molds and may just be called amerospores in the lab report.
But when these spores appear in spore chains (as that's how they are born) they should not be labeled as amerospores, and at least some of these airborne spores in the Aspergillus/Penicillium group can be identified from the spore alone (such as Aspergillus niger).
Above at left we're examining an Aspergillus fumigatus conidiophore from a top-down view. The Aspergillus fumigatus conidiophore is the spore-producing structure and as you can see spores are produced in dense profusion and in long chains.
Above at right we illustrate a quite dense building-surface growth of Aspergillus niger and Aspergillus fumigatus side by side, in the same surface sample, but not quite intermixed. These spores were collected by a tape lift sample. The colorless spores in the open area may be another species of Aspergillus or of Penicillium.
See MOLD APPEARANCE - WHAT MOLD LOOKS LIKE for images of what mold looks like when growing on building surfaces or materials.
A thumbnail Sketch about Aspergillosis-related Illnesses and Aspergillus fumigatus.
List of Aspergillus-mold-related illnesses
The following is excerpted
from MOLD RELATED ILLNESS SYMPTOMS
- Allergic Bronchiopulmonary Aspergillosis (ABPA) - worsening of underlying asthma or cystic fibrosis, coughing up blood, weight loss, fever, wheezing, mucous plugs produced by coughing - uncommon, occurs in persons with asthma and those with cystic fibrosis (CF).
- Aspergilloma (fungal growth in lung), cough, cough, fever, weight loss. Uncommon. May be asymptomatic but show up in a lung X-ray in some patients who have a pre-existing lung cavity (e.g. due to T.B.), occurs in patients suffering HIV + pneumonia; coughing up blood is a serious and life threatening condition.
- Aspergillosis, Chronic necrotizing Aspergillus pneumonia, or Chronic necrotizing pulmonary aspergillosis (CNPA) occurs in patients with an underlying disease such as COPD or alcoholism, symptoms include sub acute pneu7monia, fever, cough, night sweats, weight loss.
- Aspergillosis, Invasive, occurs in patients who suffer from immunosuppression or prolonged neutropenia, leukemia, and others; symptoms include fever, cough, chest pain, difficulty breathing (dyspena), rapid breathing (tachypnea).
Everyone breathes in some Aspergillus spores every day, including Aspergillus fumigatus that is itself quite common in the air. In healthy people breathing in mold spores does not cause a health problem as they are breathed out, coughed-out, or handled by the individual's immune system. In people with a suppressed immune system there are however health risks from breathing in such spores.
I don’t know what test your Dad had performed nor whether or not the test that was performed distinguishes between the presence of Aspergillus spores (they can be hard to speciate) and the existence of Aspergillosis disease.
Many people have Aspergillus spores in their lungs. I do. I have exampled coughed up flem for, and found, significant levels of Aspergillus spores.
That alone does not mean that a person has Aspergillosis.
Aspergillosis is detected by a variety of means including a combination of imaging and sometimes biopsy or even surgical procedures. Under the microscope
we’d see not just spores but living, branching fungal hyphae (think “roots” or “branches” that ultimately produce as well conidiophores or spore-producing structures).
Denning (1998) notes that invasive aspergillosis was first identified as an opportunistic infection in 1958 and adds that the diagnosis of Aspergillosis has since then increased significantly. He cites four reasons for an increase in the number of poeple at risk of developing invasive aspergillosis:
- The spread of AIDS
- Increased use of chemotherapy for treatment of solid tumors, lymphoma, leukemia and myeloma
- Increase occurrence of organ transplants
- Increased use of immunosuppressive treaments for other illnesses such as lupus and erythematosus.
For those of us including myself who can be frightened by reading about Aspergillosis it is significant to note that while there are fungal diseases that can affect healthy people, those whose immune system is impaired or suppressed are at the greatest risk. Having some Aspergillus spores in your spit doesn't mean you've got Aspergillosis.
Fisher (1981) noted that:
In one year, only 9 percent of the patients with Aspergillus species isolated from the sputum had an invasive infection.
Yu (1986) points out:
One hundred and eight consecutive patients were evaluated in whom Aspergillus species were isolated from respiratory secretions. Invasive aspergillosis was not demonstrated in non-immunosuppressed patients or in patients with solid tumors in the absence of neutropenia. Lung tissue was examined in 17 patients with leukemia and/or neutropenia [few neutrophils in the blood, leading to increased susceptibility to infection.
It is an undesirable side effect of some cancer treatments - Ed.]; all had invasive aspergillosis. Tissue examination was not performed in 20 neutropenic patients; of 17 not receiving antifungal therapy, 16 died.
Aspergillosis is usually a quite serious medical problem deserving expert medical care (often treated with anti-fungal medicines, steroids, sometimes surgery). Un-treated it can be fatal.
A common species of Aspergillus found in people suffering from Aspergillosis is Aspergillus fumigatus - shown below in photos from our laboratory.
Your dad will want to discuss his medical condition with his doctor immediately and if they agree, to be referred to a pulmonologist who is a specialist in the area of fungal diseases.
I add that Aspergillosis usually affects seriously people who suffer from immune system impairment for any of a variety of reasons. In healthy people the Aspergillus spores that we inhale do not cause a medical problem.
Aspergillosis related diseases can occur in anyone (at least some of of the Aspergillus-related diseases) but affect particularly seriously people who suffer from immune system impairment for any of a variety of reasons. In healthy people the Aspergillus spores that we inhale do not normally cause a medical problem.
Why are Aspergillus and Penicillium of Particular Health Concern Inside Buildings?
Well they are and they aren't. Certainly there are other mold genera/species that can be quite harmful, pathogenic, toxic, or allergenic to humans.
But these two mold groups, in my opinion, particularly Aspergillus sp., grow happily on an enormous variety of materials that are found on or in building interiors. So do some other molds such as Stachybotrys chartarum that has taken a beating in the public media and that is often a mycotoxin-rich mold spore. Here's an important difference:
Stachybotrys chartarum is a comparatively huge spore, maybe 10 x 20 microns, and it's sticky. It evolved to be spread by sticking to a cow's foot as the cow rambled around in damp or wet straw. Bit spores are not easily airborne unless you kick them around and they tend not to be airborne in huge numbers unless you're doing a maniacal demolition of moldy drywall without dust control. Big mold spores want to get stuck in the nose of the inhaler.
Aspergillus and Penicillium spores can be as small as 1u, that's 1 micron. These teensy spores pass easily through small openings, remain airborne for a long time, are easily carried on indoor convection currents, and can be inhaled deeply into the lung.
During a building investigation for problematic levels of mold contamination (more than 30 sq. ft. deserves professional remediation) we need to look not just at the external visible surfaces but we need to be alert for the possibility of a large but hidden mold reservoir in a building ceiling or wall cavity or even in building insulation.
How do those Aspergillus spores get out to become inhaled? Building pressure changes can indeed cause air to move in and out of walls or ceilings enough that if there is a significant mold reservoir we may find it in the indoor environment even though it's not visible. And surprisingly (to those of us who are not mycologists), changes in temperature, humidity, and sometimes even barometric pressure can cause a veritable explosion of production of mold spores.
In a college library in New York and inspecting and testing both before and after a building dry-out project began, I could both measure and actually see a tremendous increase in the airborne Aspergillus sp. level in the building after a mold "remediation" company installed fans and dehumidifiers.
The drop in humidity converted a large mold reservoir on some books to a large airborne mold cloud. When the humidity level plummeted I could actually see little clouds of green Aspergillus spores swirl into the air as I walked past moldy books on shelves. The Aspergillus had been there for a while, in a damp environment. Things dried out and the Aspergillus conidiophore mommas said to their spore-babies: Hey you kids, you're outa-here! Everybody into the air, now!
Should We Cut Holes to Inspect for Mold in Ceilings or Walls?
I don't suggest running through the house with an axe, but it is worth a careful inspection for humidity or moisture traps as well as possibly hidden leaks. If I can identify one or more high risk locations in a building I'd make a small test cut to look inside the cavity.
If I cannot find any high risk locations AND if there are not building-related IAQ complaints AND if I do not find abnormal occurrences of problematic mold spores in tape samples of representative settled dust, then I have to conclude there's not sufficient evidence of an indoor resevoir to cut or dig further.
Aspergillosis Research & References
- ASPERGILLOSIS, a write-up by Eloise M. Harman and other experts and posted at emedicine.medscape.com provides a thorough review of the types of Aspergillus-related illnesses, their detection, treatment, and related information. - retrieved 15 Sept 2015, original source: http://emedicine.medscape.com/article/296052-overview
- Cornet, M., L. Fleury, C. Maslo, J-F. Bernard, G. Brücker, and Invasive Aspergillosis Surveillance Network of the Assistance Publique-Hopitaux de Paris. "Epidemiology of invasive aspergillosis in France: a six-year multicentric survey in the Greater Paris area." Journal of Hospital Infection 51, no. 4 (2002): 288-296.
Abstract
Invasive aspergillosis is the most prevalent mould infection. An epidemiological surveillance network was set up in 18 teaching hospitals in Paris and the Greater Paris area. Prospective surveillance was conducted between 1994 and 1999. Between 1994 and 1997 cases were categorized as proven or probable aspergillosis and then the European Organization for Research and Treatment of Cancer/Mycoses Study Group criteria were used.
The authors analysed 621 cases (115 proven, 506 probable). No seasonal variation was found. Haematological disorders (73%) including stem-cell transplantation (36%), solid-organ transplantations (10%) and AIDS (9%) were the main underlying conditions. The crude mortality was 63%. Incidence of IA was 8% (CI95: 6.5–9.5) in acute myelocytic leukaemia and 6.3% (CI95: 4.3–8.3) in acute lymphocytic leukaemia.
Incidence was 12.8% (CI95: 10.8–14.8) following allogeneic stem-cell transplantation and 1.1% (CI95: 0.7–1.5) following autologous stem-cell transplantation. In solid-organ recipients incidence ranged from 11% following heart–lung transplantation and small bowel to 0.4% following kidney transplantation. Incidence in HIV infected patients ranged from 0.02 to 0.13% per annum. This large series confirmed that patients with haematologic disorders and transplantations are the most at risk for IA. - Denning, David W. "Invasive aspergillosis." Clinical infectious diseases (1998): 781-803.
- Denning, David W., Jeanette Y. Lee, John S. Hostetler, Peter Pappas, Carol A. Kauffman, Daniel H. Dewsnup, John N. Galgiani et al. "NIAID Mycoses Study Group multicenter trial of oral itraconazole therapy for invasive aspergillosis." The American journal of medicine 97, no. 2 (1994): 135-144.
Abstract
Background: Invasive aspergillosis is the most common invasive mould infection and a major cause of mortality in immunocompromised patients. Response to amphotericin B, the only antifungal agent licensed in the United States for the treatment of aspergillosis, is suboptimal.
Methods: A multicenter open study with strict entry criteria for invasive aspergillosis evaluated oral itraconazole (600 mg/d for 4 days followed by 400 mg/d) in patients with various underlying conditions. Response was based on clinical and radiologic criteria plus microbiology, histopathology, and autopsy data. Responses were categorized as complete, partial, or stable. Failure was categorized as an itraconazole failure or overall failure.
Results: Our study population consisted of 76 evaluable patients. Therapy duration varied from 0.3 to 97 weeks (median 46). At the end of treatment, 30 (39%) patients had a complete or partial response, and 3 (4%) had a stable response, and in 20 patients (26%), the protocol therapy was discontinued early (at 0.6 to 54.3 weeks) because of a worsening clinical course or death due to aspergillosis (itraconazole failure). Twenty-three (30%) patients withdrew for other reasons including possible toxicity (7%) and death due to another cause but without resolution of aspergillosis (20%).
Itraconazole failure rates varied widely according to site of disease and underlying disease group: 14% for pulmonary and tracheobronchial disease, 50% for sinus disease, 63% for central nervous system disease, and 44% for other sites; 7% in solid organ transplant, 29% in allogeneic bone marrow transplant patients, and 14% in those with prolonged granulocytopenia (median 19 days), 44% in AIDS patients, and 32% in other host groups. The relapse rates among those who completed therapy and those who discontinued early for possible toxicity were 12% and 40%, respectively; all were still immunosuppressed.
Conclusion: Oral itraconazole is a useful alternative therapy for invasive aspergillosis with response rates apparently comparable to amphotericin B. Relapse in immunocompromised patients may be a problem. Controlled trials are necessary to fully assess the role of itraconazole in the treatment of invasive aspergillosis. - Fisher, Bruce D., Donald Armstrong, Bessie Yu, and Jonathan WM Gold. "Invasive aspergillosis: progress in early diagnosis and treatment." The American journal of medicine 71, no. 4 (1981): 571-577.
Abstract
Ninety-one patients with documented invasive infections due to an Aspergillus species were identified at Memorial Sloan-Kettering Cancer Center from July 1, 1971, through December 31, 1976. Of the 29 patients in whom the diagnosis was made during life, 10 had successful treatment and survived the Aspergillus infection by two to 17 months. An immunodiffusion test was useful in the early diagnosis of invasive aspergillosis, and in 11 patients in whom the diagnosis was supported by seroconversion and who underwent treatment, the survival rate was 64 percent.
Cultures of respiratory secretions were not reliable because they often reflected only colonization. In one year, only 9 percent of the patients with Aspergillus species isolated from the sputum had an invasive infection. The lung was the commonest site of involvement, 91 percent of the patients having pulmonary lesions. The most frequently affected extrapulmonary organ was the brain (18.3 percent). Eight patients had nonpulmonary aspergillosis as the only manifestation of this infection. Most of the 91 patients had hematologic neoplasms as the underlying disease, and neutropenia and antibacterial therapy preceded the diagnosis of aspergillosis in the majority of cases. - Greene, Reginald E., Haran T. Schlamm, Jörg-W. Oestmann, Paul Stark, Christine Durand, Olivier Lortholary, John R. Wingard et al. "Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign." Clinical Infectious Diseases 44, no. 3 (2007): 373-379.
Abstract
Background. Computed tomography (CT) of the chest may be used to identify the halo sign, a macronodule surrounded by a perimeter of ground-glass opacity, which is an early sign of invasive pulmonary aspergillosis (IPA). This study analyzed chest CT findings at presentation from a large series of patients with IPA, to assess the prevalence of these imaging findings and to evaluate the clinical utility of the halo sign for early identification of this potentially life-threatening infection.
Methods. Baseline chest CT imaging findings from 235 patients with IPA who participated in a previously published study were systematically analyzed. To evaluate the clinical utility of the halo sign for the early identification and treatment of IPA, we compared response to treatment and survival after 12 weeks of treatment in 143 patients who presented with a halo sign and in 79 patients with other imaging findings.
Results. At presentation, most patients (94%) had ⩾1 macronodules, and many (61%) also had halo signs. Other imaging findings at presentation, including consolidations (30%), infarct-shaped nodules (27%), cavitary lesions (20%), and air-crescent signs (10%), were less common. Patients presenting with a halo sign had significantly better responses to treatment (52% vs. 29%; P < .001) and greater survival to 84 days (71% vs. 53%; P < .01) than did patients who presented with other imaging findings.
Conclusions. Most patients presented with a halo sign and/or a macronodule in this large imaging study of IPA. Initiation of antifungal treatment on the basis of the identification of a halo sign by chest CT is associated with a significantly better response to treatment and improved survival. - Greenberger, Paul A. "Allergic bronchopulmonary aspergillosis." Journal of Allergy and Clinical Immunology 110, no. 5 (2002): 685-692.
Abstract
Allergic bronchopulmonary aspergillosis (ABPA) complicates asthma and cystic fibrosis. The survival factors in Aspergillus fumigatus that support saprophytic growth in bronchial mucus are not understood. Prednisone remains the most definitive treatment but need not be administered indefinitely. MHC II –restricted CD4+ T H2 clones have been derived from patients with ABPA.
The total serum IgE concentration is elevated sharply but is “nonspecific. ” IgE serum isotypic antibodies to A fumigatus are useful in diagnosis; this is in contrast to the situation for patients with asthma without ABPA. High-resolution computed tomography of the chest demonstrates multiple areas of bronchiectasis in most patients with ABPA and is a useful radiologic tool. Some asthma control patients might have a few bronchiectatic airways, but not to the extent seen in or of the same character as those in ABPA. This review discusses clinical, radiologic, investigational, pathogenetic, and treatment issues of ABPA. (J Allergy Clin Immunol 2002;110:685-92.) - Herbrecht, Raoul, David W. Denning, Thomas F. Patterson, John E. Bennett, Reginald E. Greene, Jörg-W. Oestmann, Winfried V. Kern et al. "Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis." New England Journal of Medicine 347, no. 6 (2002): 408-415.
- Latgé, Jean-Paul. "Aspergillus fumigatus and aspergillosis." Clinical microbiology reviews 12, no. 2 (1999): 310-350.
Abstract:
Aspergillus fumigatus is one of the most ubiquitous of the airborne saprophytic fungi. Humans and animals constantly inhale numerous conidia of this fungus. The conidia are normally eliminated in the immunocompetent host by innate immune mechanisms, and aspergilloma and allergic bronchopulmonary aspergillosis, uncommon clinical syndromes, are the only infections observed in such hosts.
Thus, A. fumigatus was considered for years to be a weak pathogen. With increases in the number of immunosuppressed patients, however, there has been a dramatic increase in severe and usually fatal invasive aspergillosis, now the most common mold infection worldwide. In this review, the focus is on the biology of A. fumigatus and the diseases it causes.
Included are discussions of (i) genomic and molecular characterization of the organism, (ii) clinical and laboratory methods available for the diagnosis of aspergillosis in immunocompetent and immunocompromised hosts, (iii) identification of host and fungal factors that play a role in the establishment of the fungus in vivo, and (iv) problems associated with antifungal therapy. - Lin, Swu-Jane, Jennifer Schranz, and Steven M. Teutsch. "Aspergillosis case-fatality rate: systematic review of the literature." Clinical Infectious Diseases 32, no. 3 (2001): 358-366. Abstract:
To update the case-fatality rate (CFR) associated with invasive aspergillosis according to underlying conditions, site of infection, and antifungal therapy, data were systematically reviewed and pooled from clinical trials, cohort or case-control studies, and case series of ⩾10 patients with definite or probable aspergillosis.
Subjects were 1941 patients described in studies published after 1995 that provided sufficient outcome data; cases included were identified by MEDLINE and EMBASE searches. The main outcome measure was the CFR. Fifty of 222 studies met the inclusion criteria. The overall CFR was 58%, and the CFR was highest for bone marrow transplant recipients (86.7%) and for patients with central nervous system or disseminated aspergillosis (88.1%). Amphotericin B deoxycholate and lipid formulations of amphotericin B failed to prevent death in one-half to two-thirds of patients.
Mortality is high despite improvements in diagnosis and despite the advent of newer formulations of amphotericin B. Underlying patient conditions and the site of infection remain important prognostic factors. - Marr, Kieren A., Michael Boeckh, Rachel A. Carter, Hyung Woo Kim, and Lawrence Corey. "Combination antifungal therapy for invasive aspergillosis." Clinical infectious diseases 39, no. 6 (2004): 797-802.
- Meyer, Richard D., Lowell S. Young, Donald Armstrong, and Bessie Yu. "Aspergillosis complicating neoplastic disease." The American journal of medicine 54, no. 1 (1973): 6-15.
Abstract
From 1964 to June 1971, 93 cases of aspergillosis were encountered at Memorial Sloan-Kettering Cancer Center. The 29 cases diagnosed in 1969–1970 and the 15 cases diagnosed in the first half of 1971 represented, respectively, a doubling and a quadrupling since 1964–1965. The incidence of aspergillosis in patients with leukemia was seven times greater than in patients with Hodgkin's disease or lymphoma (p < 0.0005). By the first half of 1971, 41 per cent of the patients who died with acute leukemia had evidence of aspergillosis.
Fourteen patients with solid tumors resembled patients with leukemia or lymphoma in that they had at least two of the following in common: corticosteroid treatment, cytotoxic therapy and leukopenia (less than 4,000 cells/mm3). Pulmonary involvement was present in 90 of 93 cases, disseminated disease in 23. The commonest clinical pattern was unremitting fever and development of pulmonary infiltrates despite broad-spectrurh antibiotic therapy. In an increasing number of cases aspergillosis followed Pseudomonas aeruginosa infections.
When present, serum aspergillus precipitins correlated well with invasive disease, but a negative test result was far less reliable. In one case of acute myelogenous leukemia the patient recovered from pulmonary aspergillosis after surgical excision of the lesion and remission of her leukemia.
The incidence of aspergillosis is increasing and should be considered in the setting of progressive pulmonary infiltrates in leukemic and other heavily immunosuppressed patients who respond poorly to antibacterial therapy. Earlier diagnosis may lead to more effective therapy. - Patterson, Thomas F, George R. Thompson, III, David W. Denning, Jay A. Fishman, Susan Hadley, Raoul Herbrecht, Dimitrios P. Kontoyiannis, Kieren A. Marr, Vicki A. Morrison, M. Hong Nguyen, Brahm H. Segal, William J. Steinbach, David A. Stevens, Thomas J. Walsh, John R. Wingard, Jo-Anne H. Young, John E. Bennett PRACTICE GUIDELINES FOR THE DIAGNOSIS AND MANAGEMENT OF ASPERGILLOSIS: 2016 UPDATE BY THE INFECTIOUS DISEASES SOCIETY OF AMERICA [PDF] retrieved 2019/10/09 original source: https://academic.oup.com/cid/article/63/4/e1/2595039
Abstract:
It is important to realize that guidelines cannot always account for individual variation among patients. They are not intended to supplant physician judgment with respect to particular patients or special clinical situations.
IDSA considers adherence to these guidelines to be voluntary, with the ultimate determination regarding their application to be made by the physician in the light of each patient's individual circumstances. aspergillosis, invasive aspergillosis, allergic aspergillosis, chronic aspergillosis, fungal diagnostics, azoles, echniocandins, amphotericin Topic: amphotericin bantifungal agentsaspergillosisaspergillusinfectiondiagnosisvoriconazole Issue Section: IDSA Guideline - Patterson, Thomas F., William R. Kirkpatrick, Mary White, John W. Hiemenz, John R. Wingard, Bertrand Dupont, Michael G. Rinaldi, David A. Stevens, John R. Graybill, and P Aspergillus Study Group. INVASIVE ASPERGILLOSIS DISEASE SPECTRUM, TREATMENT PRACTICES, AND OUTCOMES [very large PDF] Medicine 79, no. 4 (2000): 250-260.
Excerpts from Introduction:
Invasive aspergillosis remains a major cause of morbidity and mortality in immunosuppressed patients. Prognosis of invasive aspergillosis has in general relied on making a prompt diagnosis of infection and in administration of high doses of amphoteriin B.
... The outcome of therapy for invasive aspergillosis is dependen not only on intensive antifungal therapy but also on recovery of underlying host defense defects such as resolution of neutropenia. Therapy of invasive aspergillosis has been difficult due to dose-limiting toxicity associated with amphotericin B deoxycholate and due to the fact that other agents such as the azoles have liited utility in criticlly ill patients with invasive infecction. Itraconazole is the only noninvestigational triazole antifungal with activity against Aspergillus species, but its use has been limited due to the fact that its oral absorption is erratic in critically ill patients. A solution offering a better absorption than capsules and an intravenous formulation hae only recently recived approval for clinial use. - Pfeiffer, Christopher D., Jason P. Fine, and Nasia Safdar. "Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis." Clinical Infectious Diseases 42, no. 10 (2006): 1417-1727.
- Soubani, Ayman O., and Pranatharthi H. Chandrasekar. "The clinical spectrum of pulmonary aspergillosis." Chest Journal 121, no. 6 (2002): 1988-1999.
Abstract:
Aspergillus is a ubiquitous fungus that causes a variety of clinical syndromes in the lung, ranging from aspergilloma in patients with lung cavities, to chronic necrotizing aspergillosis in those who are mildly immunocompromised or have chronic lung disease. Invasive pulmonary aspergillosis (IPA) is a severe and commonly fatal disease that is seen in immunocompromised patients, while allergic bronchopulmonary aspergillosis is a hypersensitivity reaction to Aspergillus antigens that mainly affects patients with asthma.
In light of the increasing risk factors leading to IPA, such as organ transplantation and immunosuppressive therapy, and recent advances in the diagnosis and treatment of Aspergillus-related lung diseases, it is essential for clinicians to be familiar with the clinical presentation, diagnostic methods, and approach to management of the spectrum of pulmonary aspergillosis. - U.S. CDC, Aspergillus & ASPERGILLOSIS [PDF] U.S. Centers for Disease Control, Tel: 800-232-4636, complete article 2019, retrieved 2019/10/09 original source: https://www.cdc.gov/fungal/diseases/aspergillosis/causes.html
Excerpt: Aspergillosis is an infection caused by Aspergillus, a common mold (a type of fungus) that lives indoors and outdoors. Most people breathe in Aspergillus spores every day without getting sick. However, people with weakened immune systems or lung diseases are at a higher risk of developing health problems due to Aspergillus.
The types of health problems caused by Aspergillus include allergic reactions, lung infections, and infections in other organs. - Victor, L. Yu, Robert R. Muder, and Abbas Poorsattar. "Significance of isolation of Aspergillus from the respiratory tract in diagnosis of invasive pulmonary aspergillosis. Results from a three-year prospective study." The American journal of medicine 81, no. 2 (1986): 249-254.
Abstract
The isolation of Aspergillus species from respiratory secretions has been regarded as being of limited usefulness in the antemortem diagnosis of invasive pulmonary aspergillosis. One hundred and eight consecutive patients were evaluated in whom Aspergillus species were isolated from respiratory secretions.
Invasive aspergillosis was not demonstrated in non-immunosuppressed patients or in patients with solid tumors in the absence of neutropenia. Lung tissue was examined in 17 patients with leukemia and/or neutropenia; all had invasive aspergillosis.
Tissue examination was not performed in 20 neutropenic patients; of 17 not receiving antifungal therapy, 16 died. Multivariate statistical analysis showed that neutropenia and absence of cigarette smoking were significant predictors of invasive aspergillosis in patients with respiratory tract cultures yielding Aspergillus.
All cases of invasive aspergillosis were associated with A. fumigatus or A. flavus. The isolation of A. fumigatus or A. flavus from the respiratory tract of a patient with leukemia and/or neutropenia is highly predictive of invasive infection. Empiric amphotericin B therapy, without the necessity for tissue diagnosis, should be considered in this patient subgroup. - Walsh, Thomas J., Elias J. Anaissie, David W. Denning, Raoul Herbrecht, Dimitrios P. Kontoyiannis, Kieren A. Marr, Vicki A. Morrison et al. TREATMENT OF ASPERGILLOSIS: CLINICAL PRACTICE GUIDELINES OF THE INFECTIOUS DISEASES SOCIETY OF AMERICA [PDF] Clinical infectious diseases 46, no. 3 (2008): 327-360.
Excerpts from Executive Summary:
Aspergillus species have emerged as an important cause of life-threatening infections in immunocompromised patients. This expanding population is composed of patients with prolonged neutropenia, advanced HIV infection, and inherited immunodeficiency and patients who have undergone allogeneic hematopoietic stem cell transplantation (HSCT) and/or lung transplantation.
This document constitutes the guidelines of the Infectious Diseases Society of America for treatment of aspergillosis and replaces the practice guidelines for Aspergillus published in 2000 [1].
The objective of these guidelines is to summarize the current evidence for treatment of different forms of aspergillosis. The quality of evidence for treatment is scored according to a standard system used in other Infectious Diseases Society of America guidelines.
This document reviews guidelines for management of the 3 major forms of aspergillosis: invasive aspergillosis, chronic (and saprophytic) forms of aspergillosis, and allergic forms of aspergillosis.
Given the public health importance of invasive aspergillosis, emphasis is placed on the diagnosis, treatment, and prevention of the different forms of invasive aspergillosis, including invasive pulmonary aspergillosis, sinus aspergillosis, disseminated aspergillosis, and several types of single-organ invasive aspergillosis.
...
Reader Comments, Questions & Answers About The Article Above
Below you will find questions and answers previously posted on this page at its page bottom reader comment box.
Reader Q&A - also see RECOMMENDED ARTICLES & FAQs
Question: Desperately in need of help with Aspergillosis & Other Mold Contamination
There was a leaking pipe in my home in a wall that we couldn't see . We found out about the problem bc of water intrusion in the walk in closet on the opposite side of the shared wall .
My sons father is 38 years old and unfortunately has an inoperable brain tumor . Prior to this he experienced a significant increase of seizure activity . Immediately prior to this he had the worse seizure I have seen to date , a 3 minute long grand mal seizure resulting in facial injury and head trauma .
I called a water mitigation company and they did a two foot cut out and pulled out the tub and surround . They pulled up the carpet and found water damaged asbestos tile .
They project remained at a standstill as we waited for the asbestos testing the insurance wanted . During that time my mother started experiencing neuroconitive changes word finding difficultly, forgetfulness, mood swings, temperature intolerance , lethargy , eye sweeping , respiratory symptoms to name a few . My 6 year old who has asthma and environmental allergies started having high fever comiting lethargy , night sweats . My two year old was having night sweats . I had everyone including my two dogs evacuate the home .
I requested mold testing . The beam in my bathroom came back positive for stachyboturs , the surface testing on my mothers furniture came back possitive for aspergillosis. The aspergillosis in the air testing came back twice the amount of the outside air even after we left I disturbed for days . The air quality inspector the insurance company sent is calling this "normal " background noise as he says we shouldn't have an issue in the living room .
Even though I said they put ky mothers belongings on my living room carpet . The first company I had pulled out mold from the Sheetrock from the walls in the bathroom which I didn't know how much or how it should properly be done . There was no containment no negative pressure . I fear my entire home is contaminated .
The remediation plan was redacted to insclude HEPA sandwhich of the entire house including soft goods, couches, and carpets and says mycotoxins and VOCs should be considered .
The house wasn't tested for it and replacement of these items is not included .
I had to take a leave of absence to get everyone to all of these medical appointments and we are requested a medical disability accommodation for my partner which as been denied by his job . I have researched and learned about mycotoxins but can't find a doctor to test or treat my mom . I went as far as having my son ( who we now know has multiple mold allergies) evaluated by environmental pediatrician at an environmental clinic in the city but turns out they aren't educated about mycotoxins .
I am desperate to have my own testing for vocs and mycotoxins as I'm terribly to bring my family back into a home that is making them sick .
Any help you could provide I would appreciate. I have photos the environmental testing the remediation if you would be willing to review . I just want to make sure my family is safe . - Anonymous by private email 2022/05/30
Moderator reply: Use an onsite expert and thorough inspection to assure that problem mold or other environmental hazards have been properly removed
What follows is my OPINION based on the very limited information I have about your building and the health concerns you raise.
Mold tests: are unreliable - Unfortunately testing alone without a very thorough inspection of the extent of work and its effectiveness, would not be reliable nor effective. In particular air tests are notoriously inaccurate with four orders of magnitude variation. Knowing so little about the home and its materials and history, we can't even be confident that while you were testing for are the only or even the most important hazards there.
Testing for MVOCs is unreliable: variations in building conditions such as humidity, temperature, and variations in mold genera/species mean that building tests for MVOCs (Mold-Volatile Organic Compounds) are at risk of giving a false negative result.
Comparing indoor and outdoor Aspergillus or Penicillium spores, though commonly included in building mold tests, is misleading since the species are likely to be entirely different.
Furthermore, no air or culture test for mold is reliable if or when such testing is used alone, without an expert inspection, review of building history, occupant complaints and vulnerabilities, etc.
Instead what's required is a more thoughtful and intelligent look at the building and its history and if the work that has been done.
Halting a mold cleanup job for testing? About your mold remediation project "remaining at a standstill", in my OPINION, immune-impaired or other highly-vulnerable people (such as infant, elderly, asthatic) ought not be present in a building at all during mold remdiation and ought not return until you are comletely confident in the successful results of post mold-remediation clearance inspection and testing.
Don't need to ID the mold to remove it: And because knowing the mold genera/species doesn't change the cleanup requirements, I'm baffled about why the job stopped.
Watch out: if a mold remediation job stops for days or longer there is risk that mold contamination in the building spreads and the ultimate cost of the job will be increased. That risk is multiplied if mold-causing building water leaks or moisture problems are also ongoing.
Watch out: in my experience, some insurance companies or adjusters are so pressed to control the costs to their company that you may not receive advice that is safe for building occupants.
Watch out: if building carpets or upholstered furniture were wet or othewise mold contaminated, they can not be successfully cleaned and need to be removed.
Keep in mind that Stachybotrys sp., or Aspergillosis sp., while both are serious health concerns if present at significant levels indoors, are by no means the only molds that will be present in a water-damaged building.
Doctors treating affected people may want to know what mold genera/species were dominant in the building, but for mold remediation, knowing the genera/species do not make one bit of difference in what is needed:
Find the mold, remove it, and fix the leaks that caused it's growth in the building.
Reader follow-up: concerns for mold, asbestos, allergies, pathogens, various family members ill, multiple coplaints.
Yes that makes complete sense . That addresses a lot of my concerns . I'm fearful that the remediation plan is place might not address all of the issue. I also know we had the asbestos tile issue . My home was built in the 70s. I have no idea what other environmental dangers might be present . All I know is the manipulation of the building material and removal of the rug seems to be what triggered an exacerbation and new onset of symptoms .
I do hve the testing remediation plan and the breakdown of the contractor who is supposed to be insisting the work . I'm trying to figure out if it's best to allow this plan to move forward and then explore further after if problems persist . I'm terribly afraid to bring my family back to my house if it's unsafe and making them sick .
I have taken my mother to primary care , infectious disease , rheumatology and they all found no answers.
My 6 year old has been to asthma and allergy, ent , environmental pediatrician, pediatrician and just more referrals for gi , neurology, and neuropsychology which I have already scheduled but earliest available is months out .
I do know when I have gone back to the house and I get headaches and shaky hands if only there for a short time . I could send over everything I have if you would be willing to review and make a suggestion . I have the appraisal from when I bough the house as well if that helps with building material .
Moderator reply: remote consulting can't substitute for a serious onsite expert
Your description of conditions in the home certainly argue that it has not been adequately inspected and cleaned of mold or other indoor environmental hazards.
If you have specific question I can try to answer or can refer you to material we've already published that may be helpful.
But in solving the very serious health concerns that you have raised involving multiple peopple, you first need to find a doctor whom you trust and listen to her advice about how to best protect and treat your family members.
Trusting this to an off-site person, even someone with experience, is not sufficient nor reliable. In my experience, virtually always, when I've visited a building where there are health or safety or other building-related concerns, I found important, sometimes critical, additional information that was simply not apparent to an concerned occupant or to some others.
Reader Follow-up: expert building inspection & tests for mold, seach for appropriate doctors
Thank you so much for taking your very valuable time to respond to me and also publish free informative educational information on your site . I can't even put into words how grateful I am for people like you. I did contact almost all the resources on your list in my area that did lead me in a better direction! If they couldn't help me themselves, just like you, they took their time (out of the kindness of their heart ) to atleast answer and if they could, suggest someone who might in fact be able to put my family in a better position to hopefully return to a safe environment.
Due to this wonderful network of people I did find someone who was able to come do an in person inspection and evaluation of my home today . They did an abundance of testing and explained why it was important from a healthcare perspective just as you have done in your reply.
This particular professional happens to have 20 plus years in environmental health and microbiology, gave me an honest explanation of each test, why he thought it was warranted or not, but also ultimately said it was up to me. He spent hours at my home and truly listened to my concerns prior to beginning testing. He explained that this will be a valuable tool for physicians. He in fact could give me three suggestions of providers, that I could consult with that could possibly suited to treat my family. He identified another source of water intrusion in "my living room control" area.
The moisture level exceeded the capability of the meter. He further explained just how the testing that was done already, even if done correctly was not as extensive and too limited considering the specific medical concerns of my family. I am totally in agreement with posting and sharing my story (anonymously for now) and hope in fact it helps someone else.
However if there is someone who I could possibly help and wants to connect directly, I wouldn't be opposed if you connect us offline. Fingers crossed this leads my family a step closer to healing. - Anon 2022/06/04
Moderator Reply: examples of moisture measurement limitations & invasive inspections for mold
Thanks for your generous remarks.
I'm glad you got an experienced investigator on site.
Watch out: Remember that measuring moisture ONLY finds moisture that's present at the time of measurement.
An old leak into a building cavity can have produces a tremendous and hazardous mold reservoir even though it currently measures as "dry".
For that reason a thorough building investigation where there are complaints such as yours, probably needs some invasive inspection. I go to the "most-suspect" areas (based on building history, leak indicators, construction methods, building materials, common leak points) and make small test cuts to look into such cavities. If no problem is seen in the cavity, that doesn't reduce risk to zero but by starting with the most-suspect area we can become more-confident in our action plan for the building.
See details at HIDDEN MOLD, HOW TO FIND
and
at TEST CUTS for SAMPLING BUILDING MATERIALS
Work done previously without proper containment means there could certainly be moldy-dust contamination of building contents such as carpets, carpet padding, curtains, etc. (I often take a vacuum test of such materials.)
A doctor specializing in envrionmental medicine will know of medical tests that may be useful including tests for MVOC exposure.
In my OPINION (I am NOT expert on this point)
I'm most concerned about
- Lung and respiratory illness
- Aspergillosis - hard to detect, hard to treat
- Effect of mycotoxins on neurology and brain function
- Hypersensitivity that can follow chronic or acute mold or mvoc or mycotoxin exposure
- Effects of all of these on people who are at extra risk: elderly, infant, immune impaired, asthmatic, etc.
These are things to discuss with your doctors.
I would like to see the inspection and test report from your recent building inspection.
On 2020-11-03 by (mod) - we discovered the mold that was poisoning us
Cece
I am sorry to read of your mold related illness concerns and agree that it is definitely overwhelming.
You need to be guided by your doctor not information you find online.
Most personal items and certainly all hard-surfaced items can be cleaned of mold or other surface contaminants; there is no justification for throwing these away unless the cost of cleaning (which might be simply wiping and HEPA vacuuming) exceeds the cost of replacing the item.
MOLD DOCTORS - ENVIRONMENTAL MEDICINE should be of help to you
On 2020-11-02 by Cece Webs - We even replaced the carbon monoxide detectors
We are a family of 4 including two small children under 4 at the time we discovered the mold that was poisoning us. Top Environmental Toxicologists confirmed not only did we have off the charts levels of mold in our apt, but two of the voluminous species were mycotoxin producing which aligns to the severe illness symptoms we were presenting with.
We are also in the unlucky group with the Haplotypes that do not properly clear mold and other environmental toxins from our system.
We had every symptom you could list under mold poisoning from me coughing up blood, to recurrent double ear infections and pneumonia. Skin infections that were assumed to be eczema at the time, and sores that were presumed to be hand/foot mouth, and even an odd situation for my infant (under 1 year old), where he had open ulcerating sores but was treated as if it was staff/strep because we were not aware of the toxic environment we were breathing in until it eventually ate thru the wall and cabinets.
We all were chronically ill for a previously healthy family and knew something was wrong when we could hardly stand and were so dizzy and fatigued we would have to sit while even opening the fridge to get food out. Now looking back on it, we were a classic fit for mold toxicity, but never assumed that for one second.
We even replaced the carbon monoxide detectors when feeling fatigued to collapsing and fearing there could be a gas issue involved was not being detected. Every step we tried to resolve our active issue while never understanding the systemic one that was worsening.
My question involves the medical profession and prolonged treatment and impact to a family including small children.
(I should state we have seen top professionals in NYC including the PEHSU unit at Mt Siani which is the top NY state funded environmental health program.... their response has always been the same... remove yourself from the environment, stay out, remediate...but of course this is what was done, yet that does not resolve the situation in our views, but only prevents from continued exposure.).
My question is this, we are now 2 years out, our belongings will never be recovered and we started anew as best we could.
Being out was not an immediate resolution for us and with in 2 weeks my children were in the ER still unable to breath and nearly stopping in the night. They would throw up flem multiple times gasping for breath all night.
This took nearly 4 months to breathe soundly at night. My 3 year old had a chest X-ray and steroids but my 1 year old did not. The steroids only added to his condition and we soon stopped. This impacted us all greatly in a cognitive capacity and physically. Speech and developmentally for the children and brain fog and memory for us as adults. While all has improved, we do not feel “normal”. 2 years out with none of our belongings, and all the appointments in the world and never a new solution to accelerate improvement or prevent this from compounding damage internally.
My beta d glucagon was off the charts showing signs of “allergic pathway inflamed by aerosolized mold spores” according to my pulmonologist but this was a blood test that was done as a courtesy after knowing my family and wanting to help us but in no way was his area of expertise and was stalled afterwards as the assumption was, you’re safe, you’re out. In no way did he expect bloodwork to support invasive fungal infections as we were walking talking seemingly put together humans though that couldn’t be farther from how we felt.
My concern is that while none of us actually received antifungals, and the impact is ongoing though we hoped the medical professionals would be correct and this would all just quickly dissipate, and so now I am left wondering if these spores have been left to run a muck in our systems targeting fatty organs like the brain, etc. where do we go from here whether it’s medical professionals in NYC area or remedies at home that are both safe for children and adults, even if different methodologies.
No doctor ever wants to touch how to actually manage this, particularly for children and we are at heightened sensitivity to environmental impact of things we breathe in, not just fungi. We have had several mini-relapse situation scares where our classic symptoms all begin to return and have to do massive cleanse. We have the top Hospital grade air filters and are on Top of cleaning and ensuring moisture is managed. We have air monitors, though more fitted for basic allergens and pollutants as mycotoxins are too small to capture.
We recently all had some inflammatory coughing skin, eyes, issues and dizzy/exhaustion, and come to find the pumpkins has developed some mold. They were not old, or even cut open, but were enough to impact us and so they went out and we’ve been in cleanup mode since. It’s a far more intensified impact than anyone else and is always like a magic hunt for where is the bad air when we have these symptoms crop up.
Every time we have found some odd growth of possibly not even a mycotoxin type of old but we are so sensitive that a small juicebix popping and spoiling to mold on damp cardboard in the bottom of a pantry is enough to make our allergic symptoms kick you that worsen if we don’t sleuth out the issue. Clearly we are extremely sensitive after this massive experience two years ago, but how do we go forward.
We have progressed in so many ways but almost anything would be an improvement of rock bottom where we were. My concern is the beta d glucagon was never addressed, and we never had scans or testing on impact to organs. Mt Siani refused today do a single test, even bloodwork on the kids, though we have some testing from allergist and pulmonologist. And their neurologist still feels they are too young for a brain scan/mri even with our now 5 year olds speech and OT issues because he would have to be sedated and she doesn’t want to take the risk.
Our other child is even younger so he hasn’t even had a chest scan. What is the way forward to ensure there is not further damage going on, and that we continue to heal from this as we have a way to go before feeling okay again. (We have Aspergillus Niger and Aspergillus Versicolor as well as many other species that can do harm outside of the mycotoxin category) ** I have tried silver and considering charcoal. The kids have supplemented vitamins with fish oil and probiotics. Throughout the experience we were given antibiotics, inhalers, allergy meds, steroids, creams, eye drops, and anything else you can think of... but never antivirals, though I’ve heard they are a beast so perhaps that was not the right course of action anyway. Thanks for reading my novel and for any suggestions you may have!
On 2020-10-16 by (mod) - USDA consumer warnings guided also by chemical industry
Note to readers:
Andrew Jacobs, writing for the New York Times in September 2020, discussed he effects of lobbying by the pesticide industry of the U.S. Department of Agriculture.
Jacobs reported that in essence the USDA not only sought input from the pesticide industry when considering regulations [in our OPINION fully appropriate] but went further in seeking industry approval of the government's position - at the expense of public health.
The reporter continued:
"Although the research on agricultural fungicides is less extensive than the study of antibiotics, scientists say the same dynamic is already playing out with the antifungal compounds that are sprayed on vegetables and flowers. Researchers believe the surge in a drug-resistant lung infection called aspergillosis is associated with the pesticides, and many suspect they are behind the rise of Candida auris, a deadly fungal infection."
[Note that Aspergllosis can be very difficult to treat and can be fatal as well - Ed.]
- source: Jacobs, Andrew, "Emails Show How Pesticide Industry Swayed U.S. Stance in U.N. Talks", The New York Times, Agriculture/Health Care, 26 September 2020, p. B3.
From The New York Times: accessible online:
Emails Show How Pesticide Industry Influenced U.S. Position in Health Talks
The U.S. insisted that new international guidelines on combating drug resistance omit any mention of fungicides — a demand that the industry made but that ran counter to science.
https://www.nytimes.com/2020/09/24/health/pesticides-drug-resistance-trump-anifungals.html?smid=em-share
Supporting Research: Pesticide Use Related to Occurrence of Aspergillosis
D'mello, Jp Felix, Ann MC Macdonald, David Postel, Wilko TP Dijksma, Aude Dujardin, and Cristina M. Placinta. "Pesticide use and mycotoxin production in Fusarium and Aspergillus phytopathogens." European Journal of Plant Pathology 104, no. 8 (1998): 741-751.
Abstract Excerpt:
In particular, the issue of fungicide-resistance in relation to mycotoxin production needs to be addressed in a concerted programme of research. Additionally, the potential of breeding and selecting cultivars resistant to disease caused by toxigenic fungi needs to be exploited in a parallel search for an environmentally acceptable solution to the question of mycotoxin contamination of plant products.
Le Pape, Patrice, Rose-Anne Lavergne, Florent Morio, and Carlos Alvarez-Moreno. "Multiple fungicide-driven alterations in azole-resistant Aspergillus fumigatus, Colombia, 2015." (2016).
Satish, S., D. C. Mohana, M. P. Ranhavendra, and K. A. Raveesha. "Antifungal activity of some plant extracts against important seed borne pathogens of Aspergillus sp." Journal of Agricultural technology 3, no. 1 (2007): 109-119.
Vaezi, A., H. Fakhim, J. Javidnia, S. Khodavaisy, Z. Abtahian, M. Vojoodi, F. Nourbakhsh, and H. Badali. "Pesticide behavior in paddy fields and development of azole-resistant Aspergillus fumigatus: should we be concerned?." Journal de Mycologie Médicale 28, no. 1 (2018): 59-64.
Abstract Excerpt:
Tricyclazole as a common fungicide wildly used to control rice blast disease in the Asian country may induce azole resistance in Aspergillus fumigatus isolates. The main reason of the acquired azole resistance is probably environmental exposure through wide fungicide use in agriculture.
On 2020-03-22 by (mod)
Mike
Don't worry a bit. I'm glad to help however we can, and it's not necessary to be an English major to work with InspectApedia.com.
I don't know who told you about fruit and mulch mold nor what is that person's expertise, but in general mulch is outdoors - outdoor airborne molds would not normally explain the severe medical problems you describe.
Mold that grows on fruit, if found indoors, might be any of a great number of mold genera/species, some of which can be very serious and occasionally dangerous, particularly to someone already in weak or poor health or with respiratory illness, such as some of the specie of Aspergillus.
Aspergillosis (discussed on the page above) s a very serious fungal infection that can invade lungs, sinuses or possibly an eye, and it can be difficult to treat, especially in advanced stages or in someone who is weak and in poor health for other reasons.
However it would be unusual for the small volume of mold that might be on fruit to be sufficient in volume to make someone sick unless you stuck your finger right onto such mold and then put it in your eye or into your nose.
Most people would not eat much less fool with visibly moldy food; they ought to and probably would just throw it away.
Therefore a more-significant question is whether or not there is a dangerous mold reservoir - a larger area of mold-contaminated materials - in the home where she lived. No simple "mold test" can answer the question, but an expert can combine a thorough visual inspection, taking of history of the building's leak events or sewage backups etc, combined with the history of occupant complaints, observations, and health, along with an understanding of how and where mold grows in buildings to make a reasonable assessment of the chances that there is a mold problem that needs to be addressed.
If there's no visible mold in the home but the situation sounds serious enough the expert will go to one or more areas that are most-suspect of hidden mold such as a ceiling or wall that suffered prior leaks, and there she might make a small test opening to inspect the building cavity.
About how much time our cousin has remaining, that's not something on which I can comment (not an M.D., knowing nothing about the individual nor case, etc), but that's a fair question to ask her doctor.
Meanwhile I extend our deep sympathy to all of you suffering this added stress and sadness at what's already a difficult time for people everywhere during the Coronavirus pandemic.
On 2020-03-22 by Mike
I am sorry after the message was sent i seen how messed up it was. She went to the emergency room with a headache she had for three days. She is diabetic . They were going to give her aquadruple . She had a infection and was sent to Shan's hospital . It was a sinus infection. They ended up removing her eye, her eye socket and sinus cavity.
She had about six surgeries to scrape all they could. They finally sent her home in hospice care to basically die. We're told it was caused by mold from fruits and from mulch piles. We are all confused and shocked how quick this has happened. Her husband is going to be lost . He ask me if i could look up all i could about this and what kind of time she could have and what is he going to be dealing with her dieing .
On 2020-03-21 by Anonymous
Mike
With apology, I do not fully understand the question, but it sounds as if you have been given confusing information.
Some molds can create some illnesses, yes. But mold exposure would not directly lead to a requirement for heart bypass surgery.
First: ask your doctor or your cousin's doctor for a clear explanation in lay-person's terms that we can understand.
Second: if you worry that your home is mold-contaminated, a combination of visual inspection for visible mold and for a history of previous or current leaks can help find problem reservoirs of mold to be replaced.
See those details
at MOLD INVESTIGATION PROCEDURE TIPS
For help deciding if you need to hire someone to help you investigate for mold contamination see
MOLD / ENVIRONMENTAL EXPERT, HIRE ?
On 2020-03-21 by Mike
My cousin went to the emergency room with a headache she had for 3 days they said she had to have a quadruple bypass surgery but they found an infection which was a sinus infection a sign of Ash and she said up there for two weeks I had to take her eye out for eye socket out six operation scraping trying to get dcrape stuff out and then all the sudden they sent her home to die with hospice.
'We're just trying to figure out what happened. Shan's said it happen from mold found on fruits and from fruits and in mulch
...
Continue reading at MOLD RELATED ILLNESS SYMPTOMS or select a topic from the closely-related articles below, or see the complete ARTICLE INDEX.
Or see these
Recommended Articles
- MOLD CONTAMINATION IN BUILDINGS - home
- MOLD DETECTION & INSPECTION GUIDE
- MOLD / ENVIRONMENTAL EXPERT, HIRE ?
- MOLD INSPECTORS & MOLD TESTERS
- MOLD DOCTORS - ENVIRONMENTAL MEDICINE
- MOLD INVESTIGATION PROCEDURE TIPS
- MOLD RELATED ILLNESS GUIDE
- MOLD TEST PROCEDURES
Suggested citation for this web page
ASPERGILLOSIS at InspectApedia.com - online encyclopedia of building & environmental inspection, testing, diagnosis, repair, & problem prevention advice.
Or see this
INDEX to RELATED ARTICLES: ARTICLE INDEX to MOLD CONTAMINATION & REMEDIATION
Or use the SEARCH BOX found below to Ask a Question or Search InspectApedia
Ask a Question or Search InspectApedia
Try the search box just below, or if you prefer, post a question or comment in the Comments box below and we will respond promptly.
Search the InspectApedia website
Note: appearance of your Comment below may be delayed: if your comment contains an image, photograph, web link, or text that looks to the software as if it might be a web link, your posting will appear after it has been approved by a moderator. Apologies for the delay.
Only one image can be added per comment but you can post as many comments, and therefore images, as you like.
You will not receive a notification when a response to your question has been posted.
Please bookmark this page to make it easy for you to check back for our response.
IF above you see "Comment Form is loading comments..." then COMMENT BOX - countable.ca / bawkbox.com IS NOT WORKING.
In any case you are welcome to send an email directly to us at InspectApedia.com at editor@inspectApedia.com
We'll reply to you directly. Please help us help you by noting, in your email, the URL of the InspectApedia page where you wanted to comment.
Citations & References
In addition to any citations in the article above, a full list is available on request.
- In addition to citations & references found in this article, see the research citations given at the end of the related articles found at our suggested
CONTINUE READING or RECOMMENDED ARTICLES.
- Carson, Dunlop & Associates Ltd., 120 Carlton Street Suite 407, Toronto ON M5A 4K2. Tel: (416) 964-9415 1-800-268-7070 Email: info@carsondunlop.com. Alan Carson is a past president of ASHI, the American Society of Home Inspectors.
Thanks to Alan Carson and Bob Dunlop, for permission for InspectAPedia to use text excerpts from The HOME REFERENCE BOOK - the Encyclopedia of Homes and to use illustrations from The ILLUSTRATED HOME .
Carson Dunlop Associates provides extensive home inspection education and report writing material. In gratitude we provide links to tsome Carson Dunlop Associates products and services.